1. The potential of in vitro cell culturing for providing standardised, reliable and safe cardiomyocyte lines for the purposes of research and potential clinical applications
Cardiovascular disease is responsible for a significant proportion of morbidity and mortality in industrialised countries. The risk for development of heart disease increases steadily from a couple per cent at the age of 20 to over 20 % in people aged >65 years. According to data obtained from the WHO official webpage, cardiovascular disease is the most common cause of death among adults on a global scale (48 %), exceeding the percentages of deaths related to cancer, diabetes and chronic lung disease [WHO global mortality data]. It could only be expected that the prevalence of cardiovascular disease would continue to grow in the near future, as the average human lifespan has increased with 25-30 % in the last 100 years. Massive effort is invested worldwide into prevention of cardiovascular disease (identification of risk factors, minimisation of their impact, early detection); treatment, when the disease has already developed; prevention of complications; and increasing quality of life for the patients. Modern cardiology has at its disposal a variety of therapeutic options combining conservative treatment and surgery to achieve optimal results for the patient. Pharmaceutical science provides many newer and potentially more effective agents every year. New medicinal products, however, must undergo prolonged and rigorous testing before they reach potential patients, as the safety concerns associated with their use may outweigh the potential benefits. This happened with cerivastatin, marketed as a potent cholesterol-lowering drug from the 90-ties of the XX century and withdrawn from the European market in 2001 because of risks for severe rhabdomyolysis; and troglitazone (an antidiabetic drug, approved for sale on the British market in July 1997 and withdrawn three months later because of increased risk for severe hepatotoxicity).
Over the history of medicine, animal models have provided ample opportunities to study the physiology and the pathology of the heart and the vascular system and to try out new medicinal agents and surgical techniques. However, it may be difficult (and sometimes, even dangerous) to translate results obtained in animal models to primates and, specifically, to man. Modelling the functioning in normal and in pathological conditions of a vitally important organ, as is the heart, on primate models, may pose multiple ethical issues that are virtually impossible to overcome at present. Deliberately producing a disease phenotype in primates and humans in order to monitor the course of a disease or try out a new therapeutic approach is likely to cause needless pain and suffering and is therefore absolutely unacceptable. Cultured cardiac cells offer the opportunity for observing and analysing data about the influence of different agents on the contractile function of the heart without using living organisms as test subjects. The use of human cells to study human conditions may help to avoid at least some of the pitfalls that occur in translation of results obtained in animal models to man. Cultured cells possess great value as a model system in which to analyse the safety profile of a drug or a therapeutic regimen, or, in case of disease cell lines, the effectiveness of the particular agent in improving the functioning of the affected cells. The stimulus-response relationship is easier to monitor in cells rather than in complex living organisms and compensatory mechanisms that may suppress, mask, or augment a response may be less difficult to identify and eliminate.
Explanted cardiomyocytes (e.g. obtained by myocardial biopsies) may be maintained in specialised nutrient media. However, primary cultures of cardiomyocytes are not long-lived enough to be seriously considered for potential therapeutic uses. Freshly isolated cardiac tissue is normally viable for less than 12 hours and cultured adult cardiomyocytes may remain alive and robustly pulsating for no more than several weeks. Therefore, primary cultures of cardiac cells could not provide a steady source of cells to try out different therapeutic regimens, as their lifespan in vitro is often shorter than the length of the average therapeutic trial. Consistency in the properties of the cultured cells used for research is crucial for the establishment of reliable experimental protocols. Primary cultures of cardiomyocytes, however, may have significant culture-to-culture and batch-to-batch variance in their properties, as they originate from different organisms and are, therefore, a product of the combined action of a different genetic background and a different environment. Thus, the results may not be reproducible, although they were obtained with essentially the same cells treated with the same agents, and the analysis of the results may be complicated by a variety of unknown factors.
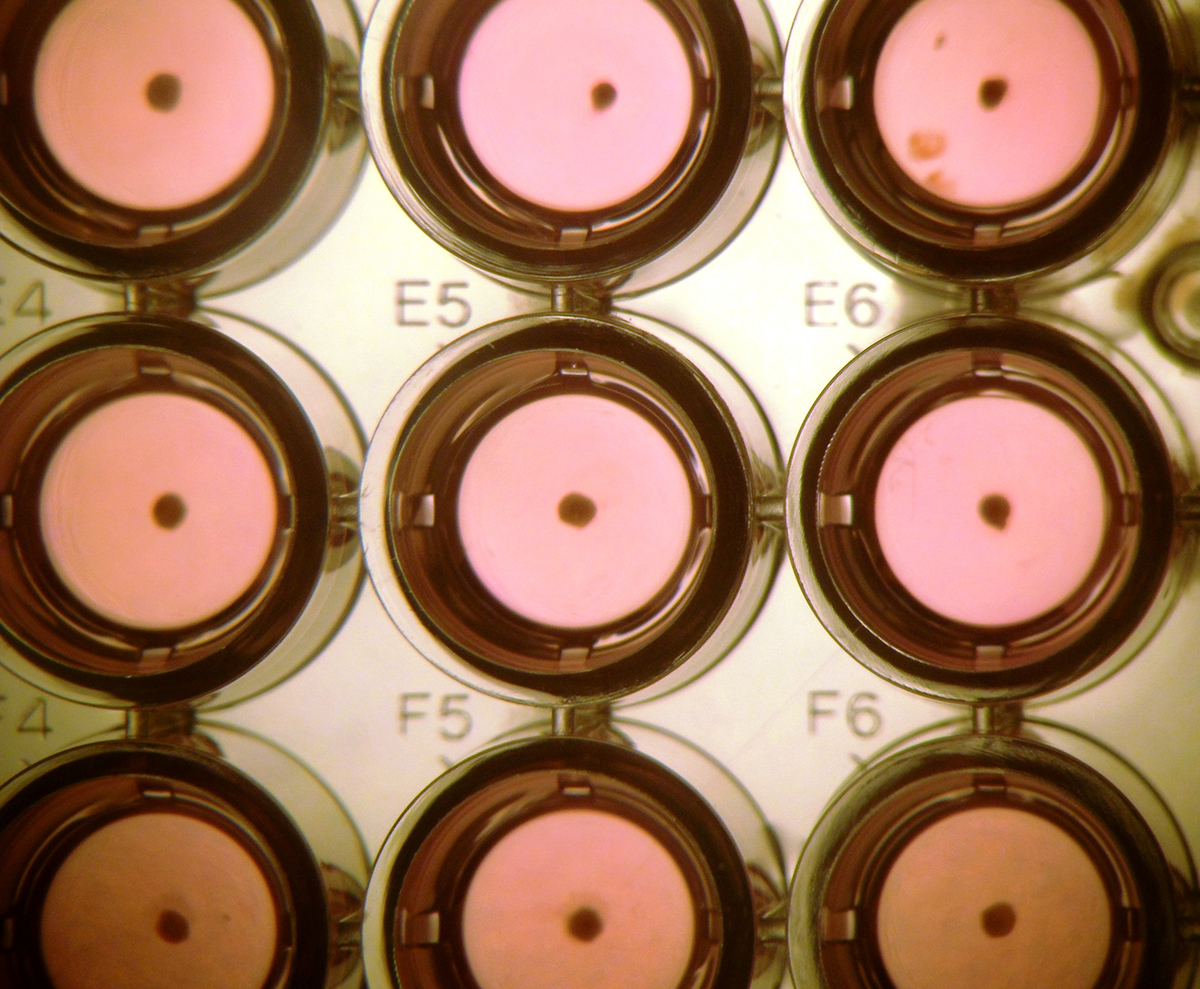
The developments in stem cell science over the last three decades provide the unique opportunity of having a virtually inexhaustible stock of high-quality cells (including human cell lines from healthy individuals as well as disease cell lines) to use in research and drug development. These cells are derived, cultured and induced into specific differentiation pathways according to standardised protocols and their properties are characterised by standardised sets of markers in order to minimise the interference of factors of unknown origin, including contact with products and substances of non-human origin such as animal feeder cells, animal sera and growth factors. Fig. 1 presents cardiomyocyte clusters cultured in vitro in xeno-free conditions in a round bottom 96-well plate.
Cultured pluripotent cell lines may be maintained in their undifferentiated state for a long time, and many batches of differentiated cells with consistent quality may be generated, maximising reliability and reproducibility of results. The use of cardiac cell lines that are derived from the same original undifferentiated cell line allows that multiple drug trials may be carried out with cells with the same basic properties, facilitating the interpretation and analysis of data. Indeed, the derivation of human embryonic stem cells (hESC) is still associated with significant ethical issues and may be restricted in some countries, but these ethical problems are on a smaller scale compared with the potential issues associated with experimentation, even with curative intent, on human beings. Fig. 2 presents a beating cardiomyocyte cluster derived in vitro from a human embryonic stem cell line.

Cardiac pacemaking, stenting, bypass surgery, valve replacement and other approaches may significantly improve the quality of life of patients with cardiovascular disease. However, there is still little to do when the function of the heart is irreversibly and severely compromised. For many decades, the main efforts in the field of care of patients with high-grade cardiac failure were targeted predominantly at improving surgical technique for heart and heart-lung transplantation, the degree of resolution of tissue compatibility typing and the establishment of larger and more representative databases for rapid and accurate donor-recipient matching. At present, transplantation of a heart taken from a deceased allogeneic donor is still the best option for patients with severe heart failure that is not treatable by any other means. However, the use of allogeneic tissues and organs of human origin are associated with specific risks. Among these risks are transmission of blood-borne infections (hepatitis viruses, human immunodeficiency virus, human T-lymphotropic virus, Epstein-Barr virus, cytomegalovirus, and the risk for immunological conflict between the transplanted tissue or organ and the recipient’s immune system. Transplantation of tissues of animal origin such as porcine or bovine bioprostheses (e.g. heart valves) may also be associated with risks of transmission of zoonotic infections (e.g. the Nipah swine virus) and, in rare cases, may cause hyperacute rejection in human recipients [
Modern cell culturing is rapidly transitioning to completely animal product-free conditions for derivation, maintenance and differentiation of human cells, eliminating the risks for transmission of infections to potential recipients and immune reactions to proteins and other compounds of animal origin. Stable lines of human cells cultured in standardised conditions may potentially provide significant opportunities in the field of regenerative medicine. It may be possible, in the not-so-distant future, to ensure that tissues and organs that have aged or have become injured because of a disease or any other reason, may be safely replaced, or, at least, that their functioning may be supported by a fresh supply of specialised cells of the same type as the damaged cells. The risks of severe immunological conflicts may also be easier to resolve with cell lines as potential sources for cells and tissues and for transplantation than with donated tissues and organs. It is believed possible that after careful analysis of the distribution of the HLA types in the particular population, the minimal set of cell lines potentially intended to produce differentiated cells for transplantation purposes may be selected specifically so that their HLA types would match with high degree of compatibility (allowing for ≤ 2 mismatches) the HLA characteristics of a significant percentage of the population [
Cultured cardiomyocytes obtained by differentiation of pluripotent cells (embryonic stem cells, induced pluripotent stem cells (iPSC)) or, possibly, by dedifferentiation/transdifferentiation from other cell types (e.g. mesenchymal stem cells (MSC) from umbilical cord) have a lot to offer to modern biomedical science. Indeed, at present the potential advantages are related predominantly to drug design and testing studies carried out in cultured cells than to their direct use for transplantation purposes. The concept of growing a new heart from cells in a culture dish still belongs to the future, but, nevertheless, it is a future much closer than it was in the XX century. This paper reviews the most commonly used protocols for targeted differentiation of pluripotent cells towards cardiogenic fate, outlining the mechanisms of action of different agents used in these protocols; the markers used for characterisation of the mesodermal and cardiogenic lineages; and summarising the specific points concerning the potential uses of cardiomyocytes derived in vitro.
2. Brief historical overview of the attempts to cultivate rhythmically beating cardiac cells under in vitro conditions
Initial attempts for establishment of primary cultures of human cardiac cells date from more than a century ago, with the experiments of the anatomist Montrose Burrows and the virtuoso surgeon Alexis Carrell [
When the first lines of embryonic stem cells were created in the 80-ties (murine embryonic stem cells, mESC) [


In 2008, three independent research groups reported the derivation of cardiomyocytes from murine iPSC using embryoid body-based and monolayer-based differentiation protocols [
3. Cardiac development in the human embryo
Pluripotent stem cells (embryonic stem cells and induced pluripotent stem cells) maintained in culture are commonly used for derivation of cardiomyocytes in vitro. The essential stages of in vitro differentiation of embryonic stem cells resembles early embryonic development, therefore, we will outline the essential points of the formation of the mammalian heart and the vascular system. The heart is the first organ to form in developing vertebrate embryos. The specification of the cardiogenic lineage occurs mainly via cell-cell interaction between the cells of the endoderm and the mesoderm [
4. Sources of stem cells capable of differentiation into cardiomyocytes
What comes from the heart goes to the heart.
S. T. Coleridge (1772 – 1834)
4.1. Adult cardiac progenitor cells
Mammalian cardiomyocytes were long considered to be cells that lasted a lifetime and, therefore, were supposedly never replaced when damaged. Indeed, heart muscle cells are very long-lived, but, similarly to the neurons in the CNS, they may be replaced, albeit at a slow rate. In 2004, cardiac progenitor cells (CPCs) were identified in mouse hearts as well as in atrial and ventricular human cardiac biopsy specimens [
in vitro, CPCs are capable of long-term self-renewal. They may differentiate into cardiomyocytes, vascular smooth muscle cells and endothelial cells in vitro as well in vivo (after transplantation into immunodeficient mice) [
In 2011, multipotent vascular stem cells (VSCs) were identified in human coronary vessels [
4.2. Cardiomyocytes produced by differentiation of multipotent adult progenitor cells other than cardiac progenitors
Some types of multipotent stem cells that usually do not produce cardiomyocyte-like cells may differentiate into cells with a cardiac phenotype. Spontaneous differentiation may occur after the cells have been transplanted in an environment providing the signals necessary for their routing towards the cardiogenic fate. Alternatively, the differentiation into the cardiogenic lineage may be guided, by supplementation with different growth factors or small molecules or by modulation of the expression of specific genes. Capacity for successful differentiation into cardiomyocytes has been demonstrated for several types of adult multipotent stem cells other than cardiac progenitor cells. Mostly, these were mesenchymal stem cells derived from umbilical cord, amniotic fluid, placenta or bone marrow [
Induced overexpression of the transcription factor myocardin was reported to result in partial transdifferentiation of mesenchymal stem cells derived from human pluripotent cells into cardiomyocytes [
Inhibition of the expression of certain genes may also promote the transdifferentiation of bone marrow mesenchymal stem cells to the cardiomyocyte lineage. Knockdown of the expression of histone deacetylase 1 (Hdac1) in rat mesenchymal stem cells from bone marrow increased the levels of expression of cardiomyocyte-related genes [
Various factors other than starting cell type may affect the outcomes of differentiation of multipotent stem cells; such are the composition of the nutrient media and the timing of the addition of supplements. For some cell types, including cardiomyocytes; mechanical stimulation may constitute a significant factor for the outcomes of differentiation. In stromal stem cells from rat bone marrow differentiated in conditions simulating increased gravity, the predominant types of specialised cells were cells that were normally subjected to sustained tensile strain (cardiomyocytes, osteocytes), whereas cells cultured in low gravity differentiated predominantly into adipocytes [
The capacity of certain types of multipotent stem cells to differentiate into cardiomyocytes in vivo has been studied intensively in recent years, albeit predominantly in animal models. Allogeneic mesenchymal stem cells have been transplanted in ischemic or infarcted myocardium of mice and pigs in the hope of improving the functioning of the heart [
Beneficial effects from transplantation of mononuclear cells from bone marrow in human patients with acute myocardial infarction have been reported in the specialised literature. The improvements were in terms of enhanced cardiac contractility and perfusion of the infarcted region; decreased myocardial inflammation and cardiomyocyte apoptosis and stimulation of neoangiogenesis [
Recently were published the results of a large double-blind study about the effects of intracardial injection of haematopoietic progenitor cells from bone marrow in perioperative settings in patients that have undergone cardiac bypass surgery [
4.3. Cardiomyocytes derived by targeted differentiation of pluripotent stem cells
4.3.1. Cardiomyocytes derived by differentiation of ESC and iPSC
The first successful attempt for derivation of cardiomyocytes from human embryonic stem cells (the H9 line, one of the commonly used in research human ES cell lines) occurred by spontaneous differentiation in embryoid bodies [
Cardiomyocytes derived from pluripotent stem cells or reprogrammed somatic cells are capable of spontaneous rhythmic contraction and generation of action potentials and ionic currents characteristic of cardiac cells. They express cardio-specific RNA and proteins and respond to agents stimulating their contractile activity such as caffeine and ryanodine. It has been reported, however, that the ‘electric phenotype’ of the cardiomyocytes obtained by differentiation of pluripotent stem cells may vary, with some cells exhibiting ‘sinus nodal-like’, ‘embryonic atrial-like’ and ‘embryonic ventricular-like’ properties [reviewed in
In 2009, cardiomyocytes and other types of specialised cells were derived from human iPSC generated by reprogramming of haematopoietic progenitors from cord blood [
Cardiomyocytes derived by targeted differentiation from iPSC also exhibit the basic properties of cardiac muscle cells, namely: propensity for spontaneous rhythmic pulsation; expression of cardio-specific RNA and proteins and capacity for response to caffeine and ryanodine [
Currently, several basic protocols for targeted differentiation of ESC and iPSC along the cardiogenic lineage have been established (for details, see below). Most of them make use, jointly or alternatively, of Activin A, bone morphogenetic proteins, Wnt signalling pathway activators, Wnt inhibitors, basic fibroblast growth factor 2 (bFGF, FGF2); vascular endothelial growth factor (VEGF), and several types of small-molecule agents such as DMSO, ascorbic acid, derivatives of vitamin D3, etc. The cardiomyocyte yield may vary from several per cent (with embryoid bodies-based protocols) to over 90 % (for monolayer cultures).
4.3.2. Cardiomyocytes derived by reprogramming of somatic cells
Functional cardiomyocytes may directly be derived from somatic cells by reprogramming. Cardiomyocyte-like cells have been generated by direct reprogramming from fibroblasts [
5. Basic types of protocols for induction of targeted differentiation along the mesodermal lineage and direction to cardiogenic fate
5.1. Nutrient media and basic supplements used for maintenance of pluripotent human cells in vitro and targeted differentiation
Targeted differentiation of pluripotent cells with the intent to produce cardiomyocytes was initally developed in spontaneously forming embryoid bodies using supplements of animal origin such as foetal serum and support substrate derived from or secreted by animal cells (e.g. gelatin, laminin or Matrigel). In its simplest version, cardiogenic induction in embryoid bodies may be carried out in DMEM medium supplemented with L-glutamine and non-essential amino acids, serum or serum replacement, beta-mercaptoethanol (an antioxidant) and bFGF, on gelatin-coated plates [
Products of animal origin and/or products with undefined composition (e.g. animal serums and Matrigel) must not come into contact with cells and cell products that may potentially be used in human beings [EudraLex - The rules governing medicinal products in the European Union, vol. 4 - Good manufacturing practice (GMP) Guidelines; http://ec.europa.eu/health/documents/eudralex/vol-4/index_en.htm]. The methodology of dispersion of colonies of undifferentiated cells and passaging also developed in the general direction of eliminating the use of enzymatic preparations (trypsin, collagenase IV, etc.). The latter are, in virtually all cases, of non-human origin (typically, bovine or porcine). Currently, methodologies for mechanical passaging are being actively developed [
At present, TeSR1 and the related mTESR1 are among the most commonly used mediums for maintenance of pluripotent stem cells in defined, feeder-free conditions. TeSR1 and mTESR1 are composed of inorganic salts, trace minerals, growth factors, saturated and unsaturated fatty acids, amino acids, proteins, vitamins, energy sources (glucose and pyruvate) and various other constituents such as antioxidants, precursors for synthesis of nucleic acids, and pH indicators [patent No. US7442548]. TeSR1 does not contain animal serum or products of animal origin. Variations exist that are less costly but may contain products of animal origin. For example, in mTeSR1, the expensive human serum albumin is substituted by bovine serum albumin and human bFGF is substituted with cloned bFGF from zebrafish [

Induction of differentiation in cultured pluripotent cells in a completely xeno-free medium usually begins with replacement of the TeSR1 medium with RPMI medium supplemented with B27. RPMI medium has several variants. Basically, it utilises a bicarbonate-based buffering system and contain the essential components listed above - inorganic salts, amino acids, vitamins, nucleotide precursors, energy sources, antioxidants, pH indicators, etc. [
Embryoid body-based methods for derivation of cardiomyocytes use specialised mediums such as APEL (albumin, polyvinyl alcohol, essential lipids) and StemPro-34 [
Monolayer protocols for induction of differentiation along the cardiogenic lineage normally use RPMI/B27 medium with Matrigel or, when completely animal-free conditions are required, synthetic products such as the Synthemax surface, providing a defined solid support for cell growth [
Timed addition of specific growth factors such as bFGF and VEGF may enhance cardiomyocyte differentiation in embryoid bodies. bFGF stimulates cell division in fibroblasts in adult tissues and plays a role in would healing and tumorigenesis. It supports the growth of human embryonic stem cells in feeder-free culturing conditions and is normally included in the medium for maintenance of pluripotent stem cells in their undifferentiated state (e.g. mTeSR1) [
5.2. Spontaneous differentiation of pluripotent stem cells along the cardiogenic lineage
Spontaneous differentiation of cultured pluripotent stem cells into beating cardiomyocytes is not unusual. A reproducible protocol for induction of spontaneous differentiation in embryoid bodies in suspension (the E9 cell line) was published first in 2001 [

5.3. Induction of differentiation by supplementation with Activin A/ bone morphogenetic protein 4 (BMP-4)
Differentiation into the cardiac line may be induced by more than one method. Typically, these methods are based on blocking potential pathways into differentiation in other than mesodermal lineage and limiting the potential of differentiation of mesoderm-committed cells towards endothelial and smooth muscle cells.
Activins and bone morphogenetic proteins (BMPs) are related to the transforming growth factor-β (TGF-β) family of proteins. Signalling associated with the maintenance of the undifferentiated state in mammalian ESC is transmitted via a TGF-β/Activin A/Nodal-dependent pathway [

The basic (4-day) protocol for induction of pluripotent human cells to differentiation along the mesodermal lineage is comprised of 24 h treatment with human recombinant Activin A followed by a 72 h treatment with BMP4 [
As BMP4 treatment may route differentiating cells towards non-mesodermal fates as well (e.g. hepatic and pancreatic specification), a second mesodermal induction protocol has been developed in order to decrease the yield of cells other than cardiomyocytes [
Another approach that may be used for increasing the percentage of differentiating cells committed to mesodermal fate is including a pretreatment phase of activation of Wnt-associated pathways [
Inclusion of additional proteins (growth factors such as bFGF and VEGF) and Wnt inhibitors such as DKK1 (dickkopf homolog 1) may enhance mesoderm differentiation and specifically differentiation along the cardiomyocyte lineage in embryoid bodies produced by the Activin A/BMP4 protocols [
5.4. Induction of differentiation into the cardiomyocyte lineage by timed Gsk3 inhibition/Wnt signalling inhibition
Wnt (Wingless/INT) ligands play important roles in two basic signalling pathways: the canonical Wnt pathway and another two pathways collectively known as non-canonical Wnt-signalling [reviewed in
Activation of the Wnt signalling pathway in vitro (e.g. by supplementing the growth medium with GSK3β - inhibitors) normally supports the maintenance of the undifferentiated state in cultured murine and human cells [
Modulation of the Wnt-associated signalling pathways in cultured pluripotent cells may, under specific conditions, be used successfully for induction of differentiation into the cardiogenic lineage. The timing of the treatment is critically important for the outcomes. Wnt/β-catenin signaling in human embryonic stem cells promotes differentiation to mesodermal lineages rather than self-renewal of the cells [
5.5. Increasing the propensity for differentiation along multiple lineages (including the cardiomyocyte lineage) by DMSO or other small-molecule agents
It has been repeatedly shown since the late 70-ties of the XX century that the presence of small amounts of DMSO (1-2 %) in the culturing medium of undifferentiated cells may induce cell differentiation. Initially, this was demonstrated with cancer cells (myeloid and lymphoid cell lines). Addition of DMSO induced reversible G1 phase arrest in human promyelocytic leukemia cell lines and B- and T-lymphoid cells [
Treatment with 1-2 % DMSO for 24-28 h was shown to increase the yield of differentiated cells originating from all three germ layers, the cardiogenic lineage included [
It has been proposed that the presence of DMSO increases the competence for differentiation in undifferentiated cells by induction of a transient G1 phase arrest [
DMSO is a commonly used cryoprotector in cell culturing, used at concentrations up to 10 %. There is always some leftover DMSO in cells that have been frozen and recently thawed. It is possible that at least part of the reported cased of spontaneously differentiating cells are related to stimulation of the differentiation pathways by the presence of DMSO in the nutrient medium.
Alpha-lipoic acid has been shown to promote DMSO-induced differentiation of mouse embryonic carcinoma cells into the cardiogenic lineage [
Ascorbic acid is a potent stimulator of the differentiation of ESC into cardiogenic fate [
Supplementation of differentiating cells with 1,25-vitamin-D3 was shown to promote differentiation along the cardiogenic lineage via negative modulation of the canonical Wnt signaling pathway and the formation of cardiomyotubes [
Other small-molecule supplements, such as 5-azacytidine, alone or in combination, may also increase the yield of cardiomyocytes from pluripotent cell lines [
6. Markers for differentiation into cardiomyocyte lineage
The presence of at least partly functional cardiomyocytes in a cell culture is easily distinguishable by a single obvious morphological sign, namely, robust spontaneous contraction. According to most protocols, it ought to be noticeable by the day 12 since the first day of induction towards differentiation.
There are markers (detectable at nucleic acids and/or protein level) that may reliably indicate onset of differentiation and the phase of differentiation along the mesodermal and the cardiogenic lineage. Undifferentiated human cells express at high level the pluripotency markers OCT4, SOX2 and NANOG, the cell surface markers stage-specific antigen-4 (SSEA4) and TRA-1-60; and alkaline phosphatase [
The cell surface marker stage-specific antigen-1 (SSEA1, LeX/SSEA1/CD15 ) is typically not expressed in hESC maintained in the undifferentiated state, but its expression is quickly upregulated in cells that have embarked on the differentiation route and may therefore be used as an early differentiation marker [
Cells committed to the cardiac mesoderm lineage may be conveniently identified using only four surface markers – ROR2 (receptor tyrosine kinase-like orphan receptor 2, an inhibitor of Wnt canonical signalling); CD13 (alanine aminopeptidase, an antigen commonly present on the surface of leukocytes); VEGFR (KDR) and platelet-derived growth factor receptor alpha (PDGFRα, a cell-surface receptor for PDGF - A, B, and C) [
Even the most effective methods for targeted differentiation into the cardiogenic lineage do not produce pure cardiomyocyte populations, but a mixture of cardiomyocytes and other cells, including undifferentiated cells. The latter may be a source of serious trouble in potential clinical applications, as transplanted cells with high proliferative potential may produce rapidly growing tumours. Thus, the cardiomyocyte-rich population obtained by targeted differentiation needs to be purified before use. Markers specific for cardiac tissue may be used for identification of differentiated cardiomyocytes such as cardiac troponin T and I, cardiac alpha-myosin heavy chain, atrial natriuretic factor, and the cardiac transcription factors GATA-4, NKX2.5, and MEF-2 [
In 2011; after screening of over 200 surface molecules, it was found that cardiomyocytes derived from human ESC or human iPSC may be identified with high specificity by the surface expression of vascular cells adhesion molecule 1 protein (VCAM1) [
7. Potential advantages of using cultured cardiomyocytes derived by differentiation from pluripotent stem cells lines
7.1. Research on the effect of different agents and different therapeutic regimens on the contractile function of the heart
There are significant advantages to using cardiac cells grown by differentiation from pluripotent cells or by reprogramming/transdifferentiation from other types of cells in studies of the effect of different agents on the human heart. Studying the effect of any agent on cultured cells, of course, is not quite the same as studying it in a complex organism. It might be, however, the next best thing, when it comes to experiments on vital organs and systems. Experimentation with therapeutic regimens that affect the functioning of the heart of human subjects and human-like primates is not acceptable, except in cases when the safety of the experiment and the potential benefits for the patient were repeatedly demonstrated in previous trials on other model systems. Thanks to the achievements of modern research and molecular diagnostics it is now possible that even minute changes representing a response to drugs affecting the functioning of cultured cells may be detected in real time. Thus, after extrapolation, the potential effects of the agent on tissue and organ level may be anticipated with a reasonable level of certainty and without risk for causing irreversible damage to patients or volunteers.
The supply of cardiomyocytes obtained by differentiation from ESC or iPSC is, at least in theory, virtually inexhaustible. Provided that the original cell line is managed in its undifferentiated state (preserving its replicative capacity as well as its differentiation potential) and that the differentiation is carried out according to the standardised protocols, the cells used for every experiment would be essentially the same as in previous experiments. Reproducibility (consistency) of results is a very important factor in research (for details, see below). Obtaining consistent results with the same cell line and between cell lines treated with the same agent or regimen increases the likelihood that the signals generated in response to the agent or the regimen were truly product of the experiment procedure and not artefacts brought by a fluctuation in the experimental conditions.
7.2. Animal and human biology may sometimes be very dissimilar
7.2.1. Animals do indeed make us human
Non-primate animals (mice and rats, rabbits, dogs, sheep, swine, and others) have been used for studying the functions of mammalian body for centuries, and, in the last several decades, for modelling human biology in physiological and pathological conditions. Even the most promising trials conducted on animals, however, may sometimes produce results that are not directly applicable (or may even be drastically different) from the results obtained when the same agent is used in human beings. It is sufficient to mention the infamous phase III clinical trial of the neuroprotector PBT that was shown to be very effective in prevention of spreading of brain damage after stroke in many animal species, but did not exhibit detectable activity when tested in human patients [
However close non-primate mammalian species might be to man with respect to their DNA sequence and chromosome structure, they may not always constitute adequate models. Apparently, there may be small but very significant differences between the physiology, the metabolism and the molecular mechanisms of basic cellular processes between animals and man. For example, the cardiovascular system of swine is similar to the cardiovascular system in humans with regard to size and internal organisation of the heart, its pumping capacity and the pulse rate (slower than in most medium-sized animals and close to normal human heart rate) [reviewed in
7.2.2. Disease-specific human stem cell lines get as close as possible to modelling human disease
The signals generated by a living model in response to external stimuli, even under strictly controlled experimental conditions, may be different in a human being affected with a certain disease or condition and in animal models of the same disease or condition. When modelling human disease in lower mammalian species, the associated signs and symptoms and the objective pathological changes may be different between humans and animals. This is specifically true when these changes affect the functioning of the central nervous system, but differences may surface in modelling disease of virtually all organs and systems in animals. In such cases, human and primate disease cell lines may be of great value, as they may provide direct insight into the molecular mechanisms underlying the disease process, meaning that the effects of the studied agents and therapeutic regimens may be observed without being masked or compensated for by other effects that occur in living organisms. This is as close as possible to modelling pathology of diseased human tissues and organs, albeit the effects of the integrative relationship at system and organism level may be lost in research in cultured cells. It is believed that disease cell lines may greatly facilitate drug development and accelerate the trials of various therapeutic agents, at the same time minimising the inherent risk of causing damage to human patients because of potential adverse effects.
The first human disease cell lines were derived from embryos with known genetic defects (usually, confirmed by preimplantation diagnostics and therefore deemed unfit for use for reproduction purposes). At present, much effort is invested into creating iPSC lines derived from reprogramming of somatic cells or progenitor cells (e.g. cells from umbilical cord or adult stem cells such as haematopoietic progenitors from bone marrow) from individuals with specific genetic backgrounds that may be associated with high risk for development of disease (patient-specific disease cell lines). Several years ago the number of established human disease cell lines was in the order of several dozens, but the number of lines available for research has grown exponentially since [summarised in
7.2.3. The Methuselah of mice – modelling reliably common multifactorial diseases and conditions on a short-living animal model is hardly likely
There is a specific issue in the area of modelling human diseases and conditions that are associated with ageing, on animals. These are conditions that typically occur late in human life (as is cardiovascular disease); and/the occurrence of which is dependent on the accumulation of events over many years (as are normal and pathological ageing of tissues and organs and cancer). Most routinely used laboratory animals are much shorter-lived than man. Mice and rats rarely live over 3 years, even in optimal conditions. Domesticated dogs and cats, depending on the breed, may live for 10-15 years, rarely longer. The average life expectancy of sheep and swine is in the same order. In contrast, higher primates have an average life expectancy of 5-6 decades in captivity and humans of today are expected to live at least 80 years. Indeed, the life cycle programming of virtually all eukaryotes currently living on Earth includes ageing and ‘death of old age’, but the difference between animal and human life expectancies may make some of the characteristics of ‘diseases of old age’ very different between animals and humans. For example, ‘diseases of old age’ (cardiovascular disease, lung disease, glucose intolerance of the elderly, joint disease, senile cataract, etc.) in short-living animals may not be associated with simple ‘wear and tear’ of tissues and organs occurring after many years of use. The DNA sequence, the gene content, the structure of the genome; the organisation and the functioning of the tissues and the organs of the man and the most commonly used laboratory animal - the mouse - are remarkably similar to one another to explain why the one species lives 20-30-times longer than the other. It is likely that the crucial differences are at molecular level and, therefore, reflect on multiple aspects of animal and human biology.
Cardiovascular damage (related to cardiac hypoxia, ischemia, etc.) and cerebrovascular damage (e.g. in stroke) is accompanied with significant increase in the amount of oxidative DNA damage. In the vicinity of the lesion site, the rate of DNA repair and the rate of apoptotic cell death in cells that had sustained irreparable damage play crucial role in the development of pathological changes in the affected tissue and the subsequent recovery. Rodents are known for their unique pattern of DNA repair, targeting the repair efforts predominantly towards the transcribed regions of the genome, whereas damage in untranscribed regions may be left unrepaired (popularly called ‘the rodent repairadox’) [
Considering this, cultured human cells are likely to provide more valuable information than animal models. Cultured cardiomyocyte progenitors (cardiac progenitor cells, vascular stem cells) and cardiomyocytes derived from pluripotent cells could be maintained in vitro for years, and, potentially, for decades. Unlike differentiated adult cardiomyocytes that are replaced (albeit at a rate of 5-10 % per decade), cardiomyocyte progenitors were programmed to last throughout a normal human life, as they have been found in hearts of nonagenarians [
7.3. A matter of consistency - one cannot evaluate results of research adequately without standardising the conditions for derivation, maintenance and targeted differentiation of stem cell lines
Much effort has been invested in making work with stem cells reproducible – that is, making possible that independent research groups may obtain consistent results with the same cells by treating them with the same compounds and under the same conditions. At present, however, different stem cell lines still may show remarkably dissimilar properties with regard to differentiation into various types of specialised cells. This prompted some authors to introduce the term ‘lineage scorecard’, assessing the potential for differentiation of a stem cell line to specific lineages or specific cell types [
The low yield of robustly beating cardiomyocytes was initially believed to be related to the use of compounds with undefined or varying composition (bovine fetal serum; animal hormones and growth factors, extracellular matrix secreted by animal cells (e.g. Matrigel) and other products of xenotic origin). Batch-to-batch variations have been reported in the specialised literature and selection of a ‘batch that works’ has been a standard instruction in the early days of stem cell culturing. Indeed, this might have been a part of the problem, but the use of products of animal origin becomes more and more limited in modern research and cells grown in completely cell-free conditions are often reported to exhibit the same unsatisfactory differentiation rates as the same cell lines grown in medium supplemented with animal serum [reviewed in
Consistency in the quality of the product is crucially important in manufacture of medicinal products that are likely to be used in humans, including cell and tissue preparations [EudraLex - The rules governing medicinal products in the EU, vol. 4 - GMP Guidelines]. Use of fully defined nutrient media and support substrates only is specifically indicated for products that may potentially be used in human beings. This is related to safety concerns about the possibility of introduction of undesired proteins and DNA of animal origin in the cell preparation that may interfere with the properties of the cells or may cause adverse reactions. New techniques for extraction and propagation of stem cells in culture have been developed that exclude any products of xenotic origin [
8. Conclusion
At present, there are several well-developed approaches for differentiation of pluripotent stem cells and reprogramming of other types of cells along the cardiomyocyte lineage - the spontaneous differentiation method (augmented by small molecules, such as DMSO), the Activin A/BMP4 method and the Wnt signalling modulation method. Components of the one methodology may be included in the other (e.g. GSK3 inhibitor pretreatment typical of the Wnt signalling modulation protocol may be included in the Activin A/BMP4 protocol). The yield of robustly beating cells expressing cardio-specific RNAs and proteins may vary from several per cent (usually, in embryoid bodies-based protocols) to 70-90 % when the basic induction protocols are complemented by supplementation with small molecules such as DMSO, ascorbic acid, 5-azacytidine, etc. or, in the case of for the Activin A/BMP4 protocols, with a second 1-day induction. Still, there are inconsistencies between the results obtained by the different research groups working with the same protocols but with different cell lines and sometimes between experiments carried out with the same cell line. Standardisation of protocols and introduction of defined and xeno-free conditions for derivation, maintenance and targeted differentiation of pluripotent and multipotent cells into functional cardiomyocytes would result in higher reproducibility of results between experiments and between laboratories. The opportunity for testing new drugs and new therapeutic regimens on differentiated human cells instead of animal models would allow for safer, more rapid and more precise analysis of the effects of a specific agent or a regimen potentially intended for human use. In the long-term, consistency in the quality of the stem cell lines used for production of differentiated cells for clinical purposes may assist in the development of a more effective system for donor-recipient matching, possibly resulting in higher success rate of clinical applications.
Acknowledgements
This research was supported by Grant No. DFNI-B01/2 at the National Science Fund, Ministry of Education and Science of Republic of Bulgaria. NZ has received financial support from Northwood Charitable Trust, Scotland.
References
- Puckett FA, Stahlfeld KR, DiMarco RF. Hyperacute rejection of a bovine pericardial prosthesis. Tex Heart Inst J 2006;33:260-261.
- Taylor CJ, Bolton EM, Pocock S, Sharples LD, Pedersen RA, Bradley JA. Banking on human embryonic stem cells: estimating the number of donor cell lines needed for HLA matching. Lancet 2005;366:2019-2025.
Reference Link - Lee JE, Kang MS, Park MH, Shim SH, Yoon TK, Chung HM, et al. Evaluation of 28 human embryonic stem cell lines for use as unrelated donors in stem cell therapy: implications of HLA and ABO genotypes. Cell Transplant 2010;19:1383-1395.
Reference Link - Carrel A, Burrows MT. Cultivation of tissues in vitro and its technique. J Exp Med 1911;13:387-396.
Reference Link - Burrows MT. Rhythmical activity of isolated heart muscle cells in vitro. Science 1912;3: 90-92.
Reference Link - Carrel A. On the permanent life of tissues outside of the organism. J Exp Med 1912;15:516-528.
Reference Link - Cavanaugh MW. Pulsation, migration and division in dissociated chick embryo heart cells in vitro. J Exp Zool 1955;128:573-589.
Reference Link - Harary I, Farley B. In vitro studies of single isolated beating heart cells. Science 1960;131:1674-1675.
Reference Link - Jacobson SL. Culture of spontaneously contracting myocardial cells from adult rats. Cell Struct Funct 1977;2: 1-9.
Reference Link - Martin G. Isolation of a pluripotent cell line from early mouse embryos cultured in medium conditioned by teratocarcinoma stem cells. Proc Natl Acad Sci USA 1981;78:7634-7638.
Reference Link - Evans M, Kaufman M. Establishment in culture of pluripotential cells from mouse embryos. Nature 1981;292:154-156.
Reference Link - Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, et al. Embryonic stem cell lines derived from human blastocysts. Science 1998;282:1145-1147.
Reference Link - Kehat I, Kenyagin-Karsenti D, Snir M, Segev H, Amit M, Gepstein A, et al. Human embryonic stem cells can differentiate into myocytes with structural and functional properties of cardiomyocytes. J Clin Invest 2001;108:407-414.
Reference Link - Laflamme MA, Chen KY, Naumova AV, Muskheli V, Fugate JA, Dupras SK, et al. Cardiomyocytes derived from human embryonic stem cells in pro-survival factors enhance function of infarcted rat hearts. Nat Biotechnol 2007;25:1015-1024.
Reference Link - Zhang P, Li J, Tan Z, Wang C, Liu T, Chen L, et al. Short-term BMP-4 treatment initiates mesoderm induction in human embryonic stem cells. Blood 2008;111:1933-1941.
Reference Link - Tran TH, Wang X, Browne C, Zhang Y, Schinke M, Izumo S, et al. Wnt3a-induced mesoderm formation and cardiomyogenesis in human embryonic stem cells. Stem Cells 2009;27:1869-1878.
Reference Link - Willems E, Spiering S, Davidovics H, Lanier M, Xia Z, Dawson M, et al. Small-molecule inhibitors of the Wnt pathway potently promote cardiomyocytes from human embryonic stem cell-derived mesoderm. Circ Res 2011;109:360-364.
Reference Link - Chetty S, Pagliuca FW, Honore C, Kweudjeu A, Rezania A, Melton DA. A simple tool to improve stem cell differentiation. Nat Methods 2013;10:553-556.
Reference Link - Mauritz C, Schwanke K, Reppel M, Neef S, Katsirntaki K, Maier LS, et al. Generation of functional murine cardiac myocytes from induced pluripotent stem cells. Circulation. 2008;118:507-517.
Reference Link - Narazaki G, Uosaki H, Teranishi M, Okita K, Kim B, Matsuoka S, et al. Directed and systematic differentiation of cardiovascular cells from mouse induced pluripotent stem cells. Circulation 2008;118:498-506.
Reference Link - Schenke-Layland K, Rhodes KE, Angelis E, Butylkova Y, Heydarkhan-Hagvall S, Gekas C, et al. Reprogrammed mouse fibroblasts differentiate into cells of the cardiovascular and hematopoietic lineages. Stem Cells 2008;26:1537-1546.
Reference Link - Zhang J, Wilson GF, Soerens AG, Koonce CH, Yu J, Palecek SP, et al. Functional cardiomyocytes derived from human induced pluripotent stem cells. Circ Res 2009;104:e30-41.
Reference Link - Itzhaki I, Maizels L, Huber I, Zwi-Dantsis L, Caspi O, Winterstern A, Feldman O, Gepstein A, Arbel G, Hammerman H, Boulos M, Gepstein L. Modelling the long QT syndrome with induced pluripotent stem cells. Nature 2011;471:225-229.
Reference Link - Schultheiss TM, Xydas S, Lassar AB. Induction of avian cardiac myogenesis by anterior endoderm. Development 1995;121:4203-4214.
- Naito AT, Shiojima I, Akazawa H, Hidaka K, Morisaki T, Kikuchi A, et al. Developmental stage-specific biphasic roles of Wnt/beta-catenin signaling in cardiomyogenesis and hematopoiesis.Proc Natl Acad Sci USA 2006;103:19812-19817.
Reference Link - Klaus A, Saga Y, Taketo MM, Tzahor E, Birchmeier W. Distinct roles of Wnt/beta-catenin and Bmp signaling during early cardiogenesis. Proc Natl Acad Sci USA 2007;104:18531-18536.
Reference Link - Martin J, Afouda BA, Hoppler S. Wnt/beta-catenin signalling regulates cardiomyogenesis via GATA transcription factors. J Anat 2010;216:92-107.
Reference Link - Mascetti V, Mendjan S, Bernardo AS, Ortmann D, Pedersen RA. 58 Wnt/β-Catenin Signalling At The Heart Of Cardiogenic Mesoderm Specification. Heart 2011;97:e7.
Reference Link - Lohr JL, Martin CM, Garry DJ. Chapter 2: Cardiac Development and Congenital Cardiac disease in Coronary Heart Disease - Clinical, Pathological, Imaging, and Molecular Profiles. Zeev Vlodaver Z, Wilson RF, Garry DJ (Eds.) Springer Science + Business Media, LLC 2012, 19-42.
- Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890-1900.
Reference Link - Messina E, De Angelis L, Frati G, Morrone S, Chimenti S, Fiordaliso F, et al. Isolation and expansion of adult cardiac stem cells from human and murine heart. Circ Res 2004;95:911-921.
Reference Link - Fazel S, Cimini M, Chen L, Li S, Angoulvant D, Fedak P, et al. Cardioprotective c-kit+ cells are from the bone marrow and regulate the myocardial balance of angiogenic cytokines. J Clin Invest 2006;116:1865-1877.
Reference Link - Kattman SJ, Huber TL, Keller GM. Multipotent Flk-1+ cardiovascular progenitor cells give rise to the cardiomyocyte, endothelial, and vascular smooth muscle lineages. Dev Cell 2006;11:723-732.
Reference Link - Bergmann O, Bhardwaj RD, Bernard S, Zdunek S, Barnabé-Heider F, Walsh S, et al. Evidence for cardiomyocyte renewal in humans. Science 2009;324:98-102.
Reference Link - Kajstura J, Gurusamy N, Ogórek B, Goichberg P, Clavo-Rondon C, Hosoda T, et al. Myocyte turnover in the aging human heart. Circ Res 2010;107:1374-1386.
Reference Link - van Vliet P, Sluijter JP, Doevendans PA, Goumans MJ. Isolation and expansion of resident cardiac progenitor cells. Expert Rev Cardiovasc Ther. 2007;5:33-43.
Reference Link - Boni A, Urbanek K, Nascimbene A, Hosoda T, Zheng H, Delucchi F, et al. Notch1 regulates the fate of cardiac progenitor cells. Proc Natl Acad Sci USA 2008;105:15529-15534.
Reference Link - Di Felice V, Zummo G. Tetralogy of Fallot as a model to study cardiac progenitor cell migration and differentiation during heart development. Trends Cardiovasc Med 2009;19(4):130-135.
Reference Link - Leri A, Hosoda T, Kajstura J, Anversa P, Rota M. Identification of a coronary stem cell in the human heart. J Mol Med (Berl). 2011;89:947-959.
Reference Link - Tang Z, Wang A, Yuan F, Yan Z, Liu B, Chu JS, et al. Differentiation of multipotent vascular stem cells contributes to vascular diseases. Nat Commun 2012;3:875.
Reference Link - Brunner S, Engelmann MG, Franz WM. Stem cell mobilisation for myocardial repair. Expert Opin Biol Ther 2008;8: 1675-1690.
Reference Link - Ichim TE, Solano F, Brenes R, Glenn E, Chang J, Chan K, et al. Placental mesenchymal and cord blood stem cell therapy for dilated cardiomyopathy. Reprod Biomed Online 2008;16:898-905.
Reference Link - Pereira WC, Khushnooma I, Madkaikar M, Ghosh K. Reproducible methodology for the isolation of mesenchymal stem cells from human umbilical cord and its potential for cardiomyocyte generation.J Tissue Eng Regen Med 2008;2:394-399.
Reference Link - Xu M, Wani M, Dai YS, Wang J, Yan M, Ayub A, et al. Differentiation of bone marrow stromal cells into the cardiac phenotype requires intercellular communication with myocytes. Circulation 2004;110:2658-2665.
Reference Link - Flaherty MP, Abdel-Latif A, Li Q, Hunt G, Ranjan S, Ou Q, et al. Noncanonical Wnt11 signaling is sufficient to induce cardiomyogenic differentiation in unfractionated bone marrow mononuclear cells. Circulation 2008;117:2241-2252.
Reference Link - Maioli M, Contini G, Santaniello S, Bandiera P, Pigliaru G, Sanna R, et al. Amniotic fluid stem cells morph into a cardiovascular lineage: analysis of a chemically induced cardiac and vascular commitment. Drug Des Devel Ther 2013;7:1063-1073.
- Hida N, Nishiyama N, Miyoshi S, Kira S, Segawa K, Uyama T, et al. Novel cardiac precursor-like cells from human menstrual blood-derived mesenchymal cells. Stem Cells 2008;26:1695-1704.
Reference Link - Zhang J, Ho JC, Chan YC, Lian Q, Siu CW, Tse HF.Overexpression of myocardin induces partial transdifferentiation of human-induced pluripotent stem cell-derived mesenchymal stem cells into cardiomyocytes. Physiol Rep 2014;2:e00237.
Reference Link - Lu DF, Yao Y, Su ZZ, Zeng ZH, Xing XW, He ZY, et al. Downregulation of HDAC1 is involved in the cardiomyocyte differentiation from mesenchymal stem cells in a myocardial microenvironment. PLoS One 2014;9:e93222.
Reference Link - Karantzali E, Schulz H, Hummel O, Hubner N, Hatzopoulos A, Kretsovali A. Histone deacetylase inhibition accelerates the early events of stem cell differentiation: transcriptomic and epigenetic analysis. Genome Biol 2008;9:R65.
Reference Link - Hu G, Wade PA. NuRD and pluripotency: a complex balancing act. Cell Stem Cell 2012;10:497-503.
Reference Link - Rose RA, Jiang H, Wang X, Helke S, Tsoporis JN, Gong N, et al. Bone marrow-derived mesenchymal stromal cells express cardiac-specific markers, retain the stromal phenotype, and do not become functional cardiomyocytes in vitro. Stem Cells 2008;26:2884-2892.
Reference Link - Huang Y, Dai ZQ, Ling SK, Zhang HY, Wan YM, Li YH. Gravity, a regulation factor in the differentiation of rat bone marrow mesenchymal stem cells. J Biomed Sci 2009;16:87.
Reference Link - Sarraf CE, Otto WR, Eastwood M. In vitro mesenchymal stem cell differentiation after mechanical stimulation.Cell Prolif 2011;44:99-108.
Reference Link - Llucià-Valldeperas A, Sanchez B, Soler-Botija C, Gálvez-Montón C, et al. Physiological conditioning by electric field stimulation promotes cardiomyogenic gene expression in human cardiomyocyte progenitor cells. Stem Cell Res Ther. 2014;5:93.
Reference Link - Orlic D, Kajstura J, Chimenti S, Jakoniuk I, Anderson SM, Li B, et al. Bone marrow cells regenerate infarcted myocardium. Nature. 2001;410:701-705.
Reference Link - Shake JG, Gruber PJ, Baumgartner WA, Senechal G, Meyers J, Redmond JM, et al. Mesenchymal stem cell implantation in a swine myocardial infarct model: engraftment and functional effects. Ann Thorac Surg 2002;73:1919-1925.
Reference Link - Poncelet AJ, Hiel AL, Vercruysse J, Hermans D, Zech F, Gianello P. Intracardiac allogeneic mesenchymal stem cell transplantation elicits neo-angiogenesis in a fully immunocompetent ischaemic swine model. Eur J Cardiothorac Surg 2010; 38:781-787.
Reference Link - Chong JJ, Yang X, Don CW, Minami E, Liu YW, Weyers JJ, et al. Human embryonic-stem-cell-derived cardiomyocytes regenerate non-human primate hearts. Nature 2014;510:273-277.
Reference Link - Strauer BE, Brehm M, Zeus T, Köstering M, Hernandez A, Sorg RV, et al. Repair of infracted myocardium by autologous intracoronary mononuclear bone marrow cell transplantation in humans. Circulation 2002;106:1913-1918.
Reference Link - Lacis A, Erglis A. Intramyocardial administration of autologous bone marrow mononuclear cells in a critically ill child with dilated cardiomyopathy. Cardiol Young 2011;21:110-112.
Reference Link - Pätilä T, Lehtinen M, Vento A, Schildt J, Sinisalo J, Laine M, et al. Autologous bone marrow mononuclear cell transplantation in ischemic heart failure: a prospective, controlled, randomized, double-blind study of cell transplantation combined with coronary bypass. J Heart Lung Transplant 2014;33:567-574.
Reference Link - Timmers L, Lim SK, Hoefer IE, Arslan F, Lai RC, van Oorschot AA, et al. Human mesenchymal stem cell-conditioned medium improves cardiac function following myocardial infarction. Stem Cell Res 2011;6:206-214.
Reference Link - Kehat I, Khimovich L, Caspi O, Gepstein A, Shofti R, Arbel G, et al. Electromechanical integration of cardiomyocytes derived from human embryonic stem cells. Nat Biotechnol 2004;22:1282-1289.
Reference Link - Tomescot A, Leschik J, Bellamy V, Dubois G, Messas E, Bruneval P, et al. Differentiation in vivo of cardiac committed human embryonic stem cells in postmyocardial infarcted rats. Stem Cells 2007;25:2200-2205.
Reference Link - Shiba Y, Fernandes S, Zhu WZ, Filice D, Muskheli V, Kim J, et al. Human ES-cell-derived cardiomyocytes electrically couple and suppress arrhythmias in injured hearts. Nature 2012;489:322-325.
Reference Link - Hudson J, Titmarsh D, Hidalgo A, Wolvetang E, Cooper-White J. Primitive cardiac cells from human embryonic stem cells. Stem Cells Dev 2012;21:1513-1523.
Reference Link - Lian X, Zhang J, Azarin SM, Zhu K, Hazeltine LB, Bao X, et al. Directed cardiomyocyte differentiation from human pluripotent stem cells by modulating Wnt/β-catenin signaling under fully defined conditions. Nat Protoc 2013;8:162-175.
Reference Link - Boheler KR, Czyz J, Tweedie D, Yang HT, Anisimov SV, Wobus AM. Differentiation of pluripotent embryonic stem cells into cardiomyocytes. Circ Res 2002;91:189-201.
Reference Link - Haase A, Olmer R, Schwanke K, Wunderlich S, Merkert S, Hess C, et al. Generation of induced pluripotent stem cells from human cord blood. Cell Stem Cell 2009;5:434-441.
Reference Link - Germanguz I, Sedan O, Zeevi-Levin N, Shtreichman R, Barak E, Ziskind A et al. Molecular characterization and functional properties of cardiomyocytes derived from human inducible pluripotent stem cells. J Cell Mol Med 2011;15:38-51.
Reference Link - Pieske B, Kretschmann B, Meyer M, Holubarsch C, Weirich J, Posival H, et al. Alterations in intracellular calcium handling associated with the inverse force-frequency relation in human dilated cardiomyopathy. Circulation 1995;92:1169-1178.
Reference Link - Pieske B, Sütterlin M, Schmidt-Schweda S, Minami K, Meyer M, Olschewski M, et al. Diminished post-rest potentiation of contractile force in human dilated cardiomyopathy. Functional evidence for alterations in intracellular Ca2+ handling. J Clin Invest. 1996;98:764-776.
Reference Link - Mulieri LA, Hasenfuss G, Leavitt B, Allen PD, Alpert NR. Altered myocardial force-frequency relation in human heart failure. Circulation 1992;85:1743-1750.
Reference Link - Weisser-Thomas J, Nguyen Q, Schuettel M, Thomas D, Dreiner U, Grohé C, et al. Age and hypertrophy related changes in contractile post-rest behavior and action potential properties in isolated rat myocytes. Age (Dordr). 2007;29:205-217.
Reference Link - Zhang YM, Hartzell C, Narlow M, Dudley SC Jr. Stem cell-derived cardiomyocytes demonstrate arrhythmic potential. Circulation. 2002;106:1294-1299.
Reference Link - Jonsson MK, Duker G, Tropp C, Andersson B, Sartipy P, Vos MA, et al. Quantified proarrhythmic potential of selected human embryonic stem cell-derived cardiomyocytes. Stem Cell Res 2010;4:189-200.
Reference Link - Ieda M, Fu JD, Delgado-Olguin P, Vedantham V, Hayashi Y, Bruneau BG, et al. Direct reprogramming of fibroblasts into functional cardiomyocytes by defined factors. Cell 2010;142:375-386.
Reference Link - Maher KO, Xu C. Marching Towards Regenerative Cardiac Therapy with Human Pluripotent Stem Cells. Discov Med 2013;15:349-356.
- Ieda M, Fukuda K. Functional cardiomyocytes could therefore be directly reprogrammed from differentiated somatic cells by transduction of the three cardiac transcription factors, Gata4, Mef2c, and Tbx5. Front Biosci (Schol Ed). 2012;4:1413-1423.
Reference Link - Xu C. Turning cardiac fibroblasts into cardiomyocytes in vivo. Trends Mol Med 2012;18:575-576.
Reference Link - Song K, Nam YJ, Luo X, Qi X, Tan W, Huang GN, et al. Heart repair by reprogramming non-myocytes with cardiac transcription factors. Nature 2012;485:599-604.
Reference Link - Addis RC, Ifkovits JL, Pinto F, Kellam LD, Esteso P, Rentschler S, et al. Optimization of direct fibroblast reprogramming to cardiomyocytes using calcium activity as a functional measure of success. J Mol Cell Cardiol 2013;60:97-106.
Reference Link - Jayawardena TM, Egemnazarov B, Finch EA, Zhang L, Payne JA, Pandya K, et al. MicroRNA-mediated in vitro and in vivo direct reprogramming of cardiac fibroblasts to cardiomyocytes. Circ Res 2012;110:1465-1473.
Reference Link - Qian L, Huang Y, Spencer CI, Foley A, Vedantham V, Liu L, et al. In vivo reprogramming of murine cardiac fibroblasts into induced cardiomyocytes. Nature 2012;485:593-598.
Reference Link - Nam YJ, Song K, Luo X, Daniel E, Lambeth K, West K, et al. Reprogramming of human fibroblasts toward a cardiac fate. Proc Natl Acad Sci USA 2013;110:5588-5593.
Reference Link - Johansson BM,Wiles MV. Evidence for involvement of activin A and bone morphogenetic protein 4 in mammalian mesoderm and hematopoietic development. Mol Cell Biol 1995;15: 141- 151.
- Denning C, Allegrucci C, Priddle H, Barbadillo-Mu-oz MD, Anderson D, Self T, et al. Common culture conditions for maintenance and cardiomyocyte differentiation of the human embryonic stem cell lines, BG01 and HUES-7. Int J Dev Biol 2006;50:27-37.
Reference Link - Pal R, Khanna A.Similar pattern in cardiac differentiation of human embryonic stem cell lines, BG01V and ReliCellhES1, under low serum concentration supplemented with bone morphogenetic protein-2. Differentiation 2007;75:112-122.
Reference Link - Park Y, Choi IY, Lee SJ, Lee SR, Sung HJ, Kim JH, Yoo YD, Geum DH, Kim SH, Kim BS. Undifferentiated propagation of the human embryonic stem cell lines, H1 and HSF6, on human placenta-derived feeder cells without basic fibroblast growth factor supplementation. Stem Cells Dev 2010;19:1713-1722.
Reference Link - Jozefczuk J, Drews K, Adjaye J. Preparation of mouse embryonic fibroblast cells suitable for culturing human embryonic and induced pluripotent stem cells. J Vis Exp 2012;64:3854.
Reference Link - Zhang X, Shen MR, Xu ZD, Hu Z, Chen C, Chi YL, et al. Cardiomyocyte differentiation induced in cardiac progenitor cells by cardiac fibroblast-conditioned medium. Exp Biol Med (Maywood) 2014;239:628-637.
Reference Link - Joannides A, Fiore-Hériché C, Westmore K, Caldwell M, Compston A, Allen N, et al. Automated mechanical passaging: a novel and efficient method for human embryonic stem cell expansion. Stem Cells 2006;24:230-235.
Reference Link - Yang L, Soonpaa MH, Adler ED, Roepke TK, Kattman SJ, Kennedy M, et al. Human cardiovascular progenitor cells develop from a KDR+ embryonic-stem-cell-derived population. Nature 2008;453:524-528.
Reference Link - Elliott DA, Braam SR, Koutsis K, Ng ES, Jenny R, Lagerqvist EL, et al. NKX2-5(eGFP/w) hESCs for isolation of human cardiac progenitors and cardiomyocytes. Nat Methods 2011;8: 1037-1040.
Reference Link - Ludwig TE, Levenstein ME, Jones JM, Berggren WT, Mitchen ER, Frane JL, et al. Derivation of human embryonic stem cells in defined conditions. Nat Biotechnol 2006a;24:185-187.
Reference Link - Ludwig TE, Bergendahl V, Levenstein ME, Yu J, Probasco MD, Thomson JA. Feeder-independent culture of human embryonic stem cells. Nat Methods 2006a;3:637-646.
Reference Link - Mummery CL, Zhang J, Ng ES, Elliott DA, Elefanty AG, Kamp TJ. Differentiation of human embryonic stem cells and induced pluripotent stem cells to cardiomyocytes: a methods overview. Circ Res 2012;111:344-358.
Reference Link - Moore GE, Woods LK, Culture Media for Human Cells - RPMI 1603, RPMI 1634, RPMI 1640 and GEM1717. Tissue Culture Association Manual 1976, 3:503-508.
Reference Link - Freund C, Ward-van Oostwaard D, Monshouwer-Kloots J, van den Brink S, van Rooijen M, Xu X, et al. Insulin redirects differentiation from cardiogenic mesoderm and endoderm to neuroectoderm in differentiating human embryonic stem cells. Stem Cells 2008;26:724-733.
Reference Link - Kattman SJ, Witty AD, Gagliardi M, Dubois NC, Niapour M, Hotta A, et al. Stage-specific optimization of activin/nodal and BMP signaling promotes cardiac differentiation of mouse and human pluripotent stem cell lines. Cell Stem Cell 2011;8:228-240.
Reference Link - Lian X, Hsiao C, Wilson G, Zhu K, Hazeltine LB, Azarin SM, et al. Robust cardiomyocyte differentiation from human pluripotent stem cells via temporal modulation of canonical Wnt signaling. Proc Natl Acad Sci USA 2012;109:E1848-E1857.
Reference Link - Li Y, Powell S, Brunette E, Lebkowski J, Mandalam R. Expansion of human embryonic stem cells in defined serum-free medium devoid of animal-derived products. Biotechnol Bioeng 2005;91:688-698.
Reference Link - Levenstein ME, Ludwig TE, Xu RH, Llanas RA, VanDenHeuvel-Kramer K, Manning D, et al. Basic fibroblast growth factor support of human embryonic stem cell self-renewal. Stem Cells 2006;24:568-574.
Reference Link - Ciruna B, Rossant J. FGF signaling regulates mesoderm cell fate specification and morphogenetic movement at the primitive streak. Dev Cell 2001;1:37-49.
Reference Link - Rosenblatt-Velin N, Lepore MG, Cartoni C, Beermann F, Pedrazzini T. FGF-2 controls the differentiation of resident cardiac precursors into functional cardiomyocytes. J Clin Invest , 2005;115:1724-1733.
Reference Link - Vandervelde S, van Luyn MJ, Tio RA, Harmsen MC. Signaling factors in stem cell-mediated repair of infarcted myocardium. J Mol Cell Cardiol 2005;39:363-376.
Reference Link - Song YH, Gehmert S, Sadat S, Pinkernell K, Bai X, Matthias N, et al. VEGF is critical for spontaneous differentiation of stem cells into cardiomyocytes. Biochem Biophys Res Commun 2007;354:999-1003.
Reference Link - Xu C, Police S, Rao N, Carpenter MK. Characterization and enrichment of cardiomyocytes derived from human embryonic stem cells. Circ Res 2002;91:501-508.
Reference Link - He JQ, Ma Y, Lee Y, Thomson JA, Kamp TJ. Human embryonic stem cells develop into multiple types of cardiac myocytes: action potential characterization. Circ Res 2003;93:32-39.
Reference Link - Beattie GM, Lopez AD, Bucay N, Hinton A, Firpo MT, King CC, et al. 2005. Activin A maintains pluripotency of human embryonic stem cells in the absence of feeder layers. Stem Cells 23:489-495.
Reference Link - James D, Levine AJ, Besser D, Hemmati-Brivanlou A. TGFbeta/activin/nodal signaling is necessary for the maintenance of pluripotency in human embryonic stem cells. Development 2005;132:1273-1282.
Reference Link - Schuldiner M, Yanuka O, Itskovitz-Eldor J, Melton DA, Benvenisty N. Effects of eight growth factors on the differentiation of cells derived from human embryonic stem cells. Proc Natl Acad Sci USA 2000;97:11307-11312.
Reference Link - Valdimarsdottir G, Mummery C. Functions of the TGFbeta superfamily in human embryonic stem cells. APMIS 2005;113:773-789.
Reference Link - Burger HG, Igarashi M, Baird D, Mason T, Bardin W, McLachlan R, et al. (1988). Inhibin: definition and nomenclature, including related substances. [letter]. J Clin Endocr Metab 1988; 66:885-886.
Reference Link - Ying QL, Nichols J, Chambers I, Smith A. BMP induction of Id proteins suppresses differentiation and sustains embryonic stem cell self-renewal in collaboration with STAT3. Cell 2003;115:281-292.
Reference Link - Sharova LV, Sharov AA, Piao Y, Shaik N, Sullivan T, Stewart CL, et al. Global gene expression profiling reveals similarities and differences among mouse pluripotent stem cells of different origins and strains. Dev Biol 2007;307:446-459.
Reference Link - Xu RH, Chen X, Li DS, Li R, Addicks GC, Glennon C, et al. 2002. BMP4 initiates human embryonic stem cell differentiation to trophoblast. Nat Biotechnol 20:1261-1264.
Reference Link - Hogan BL, Blessing M, Winnier GE, Suzuki N, Jones CM. Growth factors in development: the role of TGFβ related polypeptide signalling molecules in embryogenesis. Development 1994;:53-60.
- Richter A, Valdimarsdottir L, Hrafnkelsdottir HE, Runarsson JF, Omarsdottir AR, Ward-van Oostwaard D, et al. BMP4 promotes EMT and mesodermal commitment in human embryonic stem cells via SLUG and MSX2. Stem Cells1 2014;32:636-648.
Reference Link - Paige SL, Osugi T, Afanasiev OK, Pabon L, Reinecke H, Murry CE. Endogenous Wnt/beta-catenin signaling is required for cardiac differentiation in human embryonic stem cells. PLoS One 2010;5:e11134.
Reference Link - Gouon-Evans V, Boussemart L, Gadue P, Nierhoff D, Koehler CI, Kubo A, et al. BMP-4 is required for hepatic specification of mouse embryonic stem cell-derived definitive endoderm. Nat Biotechnol 2006;24:1402-1411.
Reference Link - Rai M, Walthall JM, Hu J, Hatzopoulos AK. Continuous antagonism by Dkk1 counter activates canonical Wnt signaling and promotes cardiomyocyte differentiation of embryonic stem cells. Stem Cells Dev 2012;21:54-66.
Reference Link - Veeman MT, Axelrod JD, Moon RT. A second canon. Functions and mechanisms of beta-catenin-independent Wnt signaling. Dev Cell 2003;5:367-377.
Reference Link - Reya T, Clevers H. Wnt signalling in stem cells and cancer. Nature 2005;434:843-850.
Reference Link - Zeng X, Tamai K, Doble B, Li S, Huang H, Habas R, Okamura H, Woodgett J, He X. A dual-kinase mechanism for Wnt co-receptor phosphorylation and activation. Nature 2005;438: 873-877.
Reference Link - Kim NH, Cha YH, Kang SE, Lee Y, Lee I, Cha SY, et al. p53 regulates nuclear GSK-3 levels through miR-34-mediated Axin2 suppression in colorectal cancer cells. Cell Cycle 2013;12:1578-1587.
Reference Link - Bienz M. TCF: transcriptional activator or repressor? Curr Opin Cell Biol 1998;10:366-372.
Reference Link - Eastman Q, Grosschedl R. Regulation of LEF-1/TCF transcription factors by Wnt and other signals. Curr Opin Cell Biol 1999;11:233-240.
Reference Link - Nusse R. WNT targets. Repression and activation. Trends Genet 1999;15:1-3.
Reference Link - Bienz M, Clevers H. Armadillo/beta-catenin signals in the nucleus- proof beyond a reasonable doubt? Nat Cell Biol 2003;5:179-182.
Reference Link - Nusse R. Wnt signaling. Cold Spring Harb Perspect Biol 2012;4:a011163.
Reference Link - Cook D, Fry MJ, Hughes K, Sumathipala R, Woodgett JR, Dale TC. Wingless inactivates glycogen synthase kinase-3 via an intracellular signaling pathway which involves a protein kinase C. EMBO J 1996;15:4526-4536.
- Chen RH, Ding WV, McCormick F. Wnt signaling to β-catenin involves two interactive components. J Biol Chem 2000;275:17894-17899.
Reference Link - Sato N, Sanjuan IM, Heke M, Uchida M, Naef F, Brivanlou AH. Molecular signature of human embryonic stem cells and its comparison with the mouse. Dev Biol 2003;260:404-413.
Reference Link - Naito AT, Shiojima I, Akazawa H, Hidaka K, Morisaki T, Kikuchi A, et al. Developmental stage-specific biphasic roles of Wnt/beta-catenin signaling in cardiomyogenesis and hematopoiesis. Proc Natl Acad Sci USA 2006;103:19812-19817.
Reference Link - Davidson KC, Adams AM, Goodson JM, McDonald CE, Potter JC, Berndt JD, et al. Wnt/β-catenin signaling promotes differentiation, not self-renewal, of human embryonic stem cells and is repressed by Oct4. Proc Natl Acad Sci U S A 2012;109:4485-4490.
Reference Link - Marvin MJ, Di Rocco G, Gardiner A, Bush SM, Lassar AB. Inhibition of wnt activity induces heart formation from posterior mesoderm. Genes Dev 2001;15:316-327.
Reference Link - Chen B, Dodge ME, Tang W, Lu J, Ma Z, Fan CW, et al. Small molecule-mediated disruption of Wnt-dependent signaling in tissue regeneration and cancer. Nat Chem Biol 2009;5:100-107.
Reference Link - Minami I, Yamada K, Otsuji TG, Yamamoto T, Shen Y, Otsuka S, et al. A small molecule that promotes cardiac differentiation of human pluripotent stem cells under defined, cytokine- and xeno-free conditions. Cell Rep 2012;2:1448-1460.
Reference Link - Collins SJ, Ruscetti FW, Gallagher RE, Gallo RC. Terminal differentiation of human promyelocytic leukemia cells induced by dimethyl sulfoxide and other polar compounds.Proc Natl Acad Sci USA 1978;75:2458-2462.
Reference Link - Sawai M, Takase K, Teraoka H, Tsukada K. Reversible G1 arrest in the cell cycle of human lymphoid cell lines by dimethyl sulfoxide. Exp Cell Res 1990;187:4-10.
Reference Link - Teraoka H, Mikoshiba M, Takase K, Yamamoto K, Tsukada K. Reversible G1 arrest induced by dimethyl sulfoxide in human lymphoid cell lines: dimethyl sulfoxide inhibits IL-6-induced differentiation of SKW6-CL4 into IgM-secreting plasma cells. Exp Cell Res 1996;222:218-224.
Reference Link - Trubiani O, Ciancarelli M, Rapino M, Di Primio R. Dimethyl sulfoxide induces programmed cell death and reversible G1 arrest in the cell cycle of human lymphoid pre-T cell line. Immunol Lett 1996;50:51-57.
Reference Link - Warburton MJ, Head LP, Ferns SA, Rudland PS. Induction of differentiation in a rat mammary epithelial stem cell line by dimethyl sulphoxide and mammotrophic hormones. Eur J Biochem 1983;133:707-715.
Reference Link - Lako M, Lindsay S, Lincoln J, Cairns PM, Armstrong L, Hole N. Characterisation of Wnt gene expression during the differentiation of murine embryonic stem cells in vitro: role of Wnt3 in enhancing haematopoietic differentiation. Mech Dev 2001;103:49-59.
Reference Link - Osafune K, Caron L, Borowiak M, Martinez RJ, Fitz-Gerald CS, Sato Y, et al. Marked differences in differentiation propensity among human embryonic stem cell lines. Nat Biotechnol 2008;26:313-315.
Reference Link - Bock C, Kiskinis E, Verstappen G, Gu H, Boulting G, Smith ZD, et al. Reference maps of human ES and iPS cell variation enable high-throughput characterization of pluripotent cell lines. Cell. 2011;144:439-452.
Reference Link - Sela Y, Molotski N, Golan S, Itskovitz-Eldor J, Soen Y. Human embryonic stem cells exhibit increased propensity to differentiate during the G1 phase prior to phosphorylation of retinoblastoma protein. Stem Cells 2012;30:1097-1108.
Reference Link - Niida H, Nakanishi M. DNA damage checkpoints in mammals. Mutagenesis 2006;21:3-9.
Reference Link - Chakarov S, Russev G (2010). DNA Repair And Cell Differentiation - Does Getting Older Means Getting Wiser as Well? Biotechnol Biotechnol Eq 2010; 24:1804-1806.
Reference Link - Luo LZ, Gopalakrishna-Pillai S, Nay SL, Park SW, Bates SE, Zeng X, et al. DNA Repair in Human Pluripotent Stem Cells Is Distinct from That in Non-Pluripotent Human Cells PLoS One 2012;7:e30541.
Reference Link - Orford KW, Scadden DT. Deconstructing stem cell self-renewal: genetic insights into cell-cycle regulation. Nat Rev Genet 2008;9:115-128.
Reference Link - Bárta T, Vinarský V, Holubcová Z, Dolezalová D, Verner J, Pospísilová S, et al. Human embryonic stem cells are capable of executing G1/S checkpoint activation. Stem Cells 2010;28:1143-1152.
Reference Link - Kim Y, Deshpande A, Dai Y, Kim JJ, Lindgren A, Conway A, et al. Cyclin-dependent kinase 2-associating protein 1 commits murine embryonic stem cell differentiation through retinoblastoma protein regulation. J Biol Chem 2009;284:23405-23414.
Reference Link - Arabadjiev A, Petkova R, Momchilova A, Chakarov S, Pankov R. Of mice and men – differential mechanisms of maintaining the undifferentiated state in mESC and hESC. Biodiscovery 2012; 3:1; DOI:10.7750/BioDiscovery.2012.3.1.
Reference Link - Deng C, Zhang P, Harper JW, Elledge SJ, Leder P. Mice lacking p21CIP1/WAF1 undergo normal development, but are defective in G1 checkpoint control. Cell 1995;82:675-684.
Reference Link - Zheleva DI, McInnes C, Gavine AL, Zhelev NZ, Fischer PM, Lane DP. Highly potent p21(WAF1)-derived peptide inhibitors of CDK-mediated pRb phosphorylation: delineation and structural insight into their interactions with cyclin A. J Pept Res 2002;60:257-270.
Reference Link - Meyerson M, Harlow E. Identification of G1 kinase activity for cdk6, a novel cyclin D partner. Mol Cell Biol 1994;14:2077-2086.
- Harbour JW, Luo RX, Dei Santi A, Postigo AA, Dean DC. Cdk phosphorylation triggers sequential intramolecular interactions that progressively block Rb functions as cells move through G1. Cell 1999;98:859-869.
Reference Link - Shen X, Yang Q, Jin P, Li X. Alpha-lipoic acid enhances DMSO-induced cardiomyogenic differentiation of P19 cells. Acta Biochim Biophys Sin (Shanghai) 2014;46:766-773.
Reference Link - Takahashi T, Lord B, Schulze PC, Fryer RM, Sarang SS, Gullans SR, et al. Ascorbic acid enhances differentiation of embryonic stem cells into cardiac myocytes. Circulation 2003;107:1912-1916.
Reference Link - Cao N, Liu Z, Chen Z, Wang J, Chen T, Zhao X, et al. Ascorbic acid enhances the cardiac differentiation of induced pluripotent stem cells through promoting the proliferation of cardiac progenitor cells. Cell Res 2012;22:219-236.
Reference Link - Hlaing SM, Garcia LA, Contreras JR, Norris KC, Ferrini MG, Artaza JN. 1,25-vitamin-D3 promotes cardiac differentiation through modulation of the Wnt signaling pathway. J Mol Endocrinol 2014;53:303-317.
Reference Link - Martin-Rendon E, Sweeney D, Lu F, Girdlestone J, Navarrete C, Watt SM. 5-Azacytidine-treated human mesenchymal stem/progenitor cells derived from umbilical cord, cord blood and bone marrow do not generate cardiomyocytes in vitro at high frequencies. Vox Sang 2008;95:137-148.
Reference Link - Naeem N, Haneef K, Kabir N, Iqbal H, Jamall S, Salim A. DNA methylation inhibitors, 5-azacytidine and zebularine potentiate the transdifferentiation of rat bone marrow mesenchymal stem cells into cardiomyocytes. Cardiovasc Ther 2013;31:201-9.
Reference Link - Gao Q, Guo M, Jiang X, Hu X, Wang Y, Fan Y. A cocktail method for promoting cardiomyocyte differentiation from bone marrow-derived mesenchymal stem cells. Stem Cells Int 2014;2014:162024.
Reference Link - Abbey D, Seshagiri PB. Aza-induced cardiomyocyte differentiation of P19 EC-cells by epigenetic co-regulation and ERK signaling. Gene 2013;526:364-373.
Reference Link - Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, et al. (1998). Embryonic stem cell lines derived from human blastocysts. Science 1998;282:1145-1147.
Reference Link - Pan G, Thomson JA. Nanog and transcriptional networks in embryonic stem cell pluripotency. Cell Res 2007;17:42-49.
Reference Link - Arabadjiev B, Petkova R, Nonchev S, Chakarov S, Momchilova A, Pankov R. Derivation of Human Embryonic Stem Cell Line from Discarded IVF Morula. Compt Rend Bulg Acad Sci 2010;63:1765-1770.
- Rosner MH, Vigano MA, Ozato K, Timmons PM, Poirier F, Rigby PW, et al. A POU-domain transcription factor in early stem cells and germ cells of the mammalian embryo. Nature 1990;345:686-692.
Reference Link - Li Y, Yu W, Cooney AJ, Schwartz RJ, Liu Y. Brief report: Oct4 and canonical Wnt signaling regulate the cardiac lineage factor Mesp1 through a Tcf/Lef-Oct4 composite element. Stem Cells 2013;31:1213-1217.
Reference Link - Evseenko D, Zhu Y, Schenke-Layland K, Kuo J, Latour B, Ge S, et al. Mapping the first stages of mesoderm commitment during differentiation of human embryonic stem cells. Proc Natl Acad Sci USA 2010;107:13742-137427.
Reference Link - Cano A, Perez-Moreno MA, Rodrigo I, Locascio A, Blanco MJ, del Barrio MG, et al. The transcription factor Snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nature Cell Biol 2000;2:76-83.
Reference Link - Hoodless PA, Pye M, Chazaud C, Labbé E, Attisano L, Rossant J, et al. FoxH1 (Fast) functions to specify the anterior primitive streak in the mouse. Genes Dev 2001;15:1257-1271.
Reference Link - Takemoto T, Uchikawa M, Yoshida M, Bell DM, Lovell-Badge R, Papaioannou VE, Kondoh H. Tbx6-dependent Sox2 regulation determines neural or mesodermal fate in axial stem cells. Nature 2011:470:394-398.
Reference Link - Fretto LJ, Snape AJ, Tomlinson JE, Seroogy JJ, Wolf DL, LaRochelle WJ, et al. Mechanism of platelet-derived growth factor (PDGF) AA, AB, and BB binding to alpha and beta PDGF receptor. J Biol Chem 1993;268:3625-3631.
- Giordano FJ, Gerber H-P, Williams S-P, VanBruggen N, Bunting S, Ruiz-Lozano P, et al. A cardiac myocyte vascular endothelial growth factor paracrine pathway is required to maintain cardiac function. Proc Nat Acad Sci 2001;98:5780-5785.
Reference Link - Autiero M, Waltenberger J, Communi D, Kranz A, Moons L, Lambrechts D, et al. Role of PlGF in the intra- and intermolecular cross talk between the VEGF receptors Flt1 and Flk1. Nature Med 2003;9:936-943.
Reference Link - Mikels AJ, Nusse R. Purified Wnt5a protein activates or inhibits beta-catenin-TCF signaling depending on receptor context. PLoS Biol 2006;4:e115.
Reference Link - Ardehali R, Ali SR, Inlay MA, Abilez OJ, Chen MQ, Blauwkamp TA, et al. Prospective isolation of human embryonic stem cell-derived cardiovascular progenitors that integrate into human fetal heart tissue. Proc Natl Acad Sci USA 2013;110:3405-3410.
Reference Link - Xu RH, Ault KT JK, Park MJ, Hwang YS, Peng Y, Sredne D, et al. (1999). Opposite effects of FGF and BMP-4 on embryonic blood formation: roles of PV.1 and GATA-2. Dev Biol 1999;208:352-361.
Reference Link - Ban K, Wile B, Kim S, Park HJ, Byun J, Cho KW, et al. Purification of cardiomyocytes from differentiating pluripotent stem cells using molecular beacons that target cardiomyocyte-specific mRNA. Circulation 2013;128:1897-1909.
Reference Link - Uosaki H, Fukushima H, Takeuchi A, Matsuoka S, Nakatsuji N, Yamanaka S, et al. Efficient and scalable purification of cardiomyocytes from human embryonic and induced pluripotent stem cells by VCAM1 surface expression. PLoS One 2011;6:e23657.
Reference Link - Dubois NC, Craft AM, Sharma P, Elliott DA, Stanley EG, Elefanty AG, et al. SIRPA is a specific cell-surface marker for isolating cardiomyocytes derived from human pluripotent stem cells.Nat Biotechnol 2011;29:1011-1018.
Reference Link - Skelton RJ, Costa M, Anderson DJ, Bruveris F, Finnin BW, Koutsis K, et al. SIRPA, VCAM1 and CD34 identify discrete lineages during early human cardiovascular development. Stem Cell Res 2014;13:172-179.
Reference Link - Shuaib A, Lees KR, Lyden P, Grotta J, Davalos A, Davis SM, et al.(for the SAINT II Trial Investigators). NXY-059 for the Treatment of Acute Ischemic Stroke. N Engl J Med 2007;357:562-571.
Reference Link - Philip M, Benatar M, Fisher M, Savitz S. Methodological Quality of Animal Studies of Neuroprotective Agents Currently in Phase II/III Acute Ischemic Stroke Trials. Stroke 2009;40:577.
Reference Link - Crick SJ, Sheppard MN, Ho SY, Gebstein L, Anderson RH. Anatomy of the pig heart: comparisons with normal human cardiac structure.J Anat. 1998;193:105-119.
Reference Link - Postrach J, Bauer A, Schmoeckel M, Reichart B, Brenner P. Heart xenotransplantation in primate models. Methods Mol Biol. 2012;885:155-168.
Reference Link - Cooper DK, Hara H, Ezzelarab M, Bottino R, Trucco M, Phelps C, et al. The potential of genetically-engineered pigs in providing an alternative source of organs and cells for transplantation. J Biomed Res 2013;27:249-253.
Reference Link - Löser P, Schirm J, Guhr A, Wobus AM, Kurtz A. Human embryonic stem cell lines and their use in international research. Stem Cells 2010;28:240-246.
- Löser P, Kobold S, Guhr A, Müller FJ, Kurtz A. Scope and impact of international research in human pluripotent stem cells. Stem Cell Rev 2012;8:1048-1055.
Reference Link - Shinnawi R, Gepstein L. iPCS Cell Modeling of Inherited Cardiac Arrhythmias. Curr Treat Options Cardiovasc Med 2014;16:331.
Reference Link - Mellon I, Bhor VA, Hanawalt PC. Preferential repair of an active gene in human cells. 1986, Proc Natl Acad Sci USA 83:8878-8882.
Reference Link - Hanawalt PC. Revisiting the rodent repairadox. Environ Mol Mutagen 2001;38;89-96.
Reference Link - Röhme D. Evidence for a relationship between longevity of mammalian species and life spans of normal fibroblasts in vitro and erythrocytes in vivo. Proc Natl Acad Sci USA 1981;78:5009-5013.
Reference Link - Fergus J, Quintanilla R, Lakshmipathy U. Characterizing Pluripotent Stem Cells Using the TaqMan® hPSC Scorecard TM Panel. Methods Mol Biol. 2014 Aug 20. [Epub ahead of print]; doi: 10.1007/7651_2014_109.
Reference Link - Kehat I, Amit M, Gepstein A, Huber I, Itskovitz-Eldor J, Gepstein L. Development of cardiomyocytes from human ES cells. Methods Enzymol. 2003;365:461-473.
Reference Link - Rouhani F, Kumasaka N, de Brito MC, Bradley A, Vallier L, Gaffney D. Genetic background drives transcriptional variation in human induced pluripotent stem cells. PLoS Genet 2014;10:e1004432.
Reference Link - Crook JM, Peura TT, Kravets L, Bosman AG, Buzzard JJ, Horne R, et al. The Generation of Six Clinical-Grade Human Embryonic Stem Cell Lines. Cell Stem Cell 2007;1:490-494.
Reference Link - Vemuri MC, Schimmel T, Colls P, Munne S, Cohen J. Derivation of human embryonic stem cells in xeno-free conditions. Methods Mol Biol 2007;407:1-10.
Reference Link - Tannenbaum SE, Turetsky TT, Singer O, Aizenman E, Kirshberg S, Ilouz N, et al. Derivation of xeno-free and GMP-grade human embryonic stem cells--platforms for future clinical applications. PLoS One 2012;7:e35325.
Reference Link - Stephenson E, Jacquet L, Miere C, Wood V, Kadeva N, Cornwell G, Codognotto S, et al. Derivation and propagation of human embryonic stem cell lines from frozen embryos in an animal product-free environment. Nat Protoc 2012;7:1366-1381.
Reference Link - Martin MJ, Muotri A, Gage F, Varki A. Human embryonic stem cells express an immunogenic nonhuman sialic acid. Nat Med 2005;11:228-232.
Reference Link - Oh SK, Choo AB.Human embryonic stem cells: technological challenges towards therapy. Clin Exp Pharmacol Physiol 2006;33:489-495.
Reference Link - Arabadjiev B, Petkova R, Chakarov S, Momchilova A, Pankov R. Do we need more human embryonic stem cell lines? Biotechnol Biotechnol Eq, 2010;24:1921-1927.
Reference Link