Introduction
Human immunodeficiency virus (HIV) disease affects the entire body. Any health personnel dealing with diagnosis and treatment in humans is at risk to get infected with this dreaded disease if proper preventive guidelines are not followed. Thus it becomes imperative to be aware of the various forms of HIV manifestations.
Oral health is an important component of the overall health status in HIV infection. Awareness of the variety of oral disorders which can develop throughout the course of HIV infection and coordination of health care services between a physician and a dentist may improve the overall health of the patient. The HIV infection progresses to acquired immunodeficiency syndrome AIDS [
AIDS epidemic is increasing all over the world without any definite treatment. Antiretroviral medications can only control the progression rate of disease [
Santos et al. reported that oral lesions were common among HIV positive children and the most common lesion was pseudomembranous candidiasis. Most of the patients with oral candidiasis were suffering from severe immunosuppression, and they concluded that candidiasis and gingivitis could be considered as an indicator of the disease progression [
Since the oral manifestations of HIV infection are common and can be considered as indicators of immunosuppression, the aim of this survey was to investigate if there was a relationship between oral manifestations and the level of immunosuppression in HIV-positive patients. The results might be used as a guide in determining the immunosuppression level of HIV disease according to oral manifestations.
Materials and methods
A cross-sectional study was carried out among 125 proven HIV-positive patients showing positive ELISA and Western blot test, selected randomly from the ART centre, Wenlock Hospital, Mangalore, India. Ethical clearance was obtained from the Institutional Ethical Committee of A.B. Shetty Dental College, Nitte University. Patients were informed about the objective of the study and signed an informed consent form before oral examination.
Data including sexual habits, IV drug abuse, hemophilia, blood transfusion, addiction, other diseases, previous CD4 counts, and opportunistic systemic infections were extracted from the patient records. All patients received oral hygiene instructions. CD4 counts were determined using complete blood count and flow cytometry.
A questionnaire was completed for each patient regarding past medical history, systemic signs and symptoms, and oral manifestations. Patients were examined by an infectious disease specialist prior to dental examination. Oral cavity was inspected carefully. Intra-oral examination was performed on a dental unit using disposable dental mirrors and sterile gauze pads under appropriate lighting. Submandibular, submental and cervical lymph nodes were palpated bidigitally by the examiner. Further clinical examination using an explorer and probing with a periodontal probe were done in order to diagnose periodontal diseases. All patients were examined by similar instruments, under the same circumstances and at the same place by the single specialist to avoid the inter-examiner bias.
The oral lesions were diagnosed according to the criteria established by the EC Clearinghouse and WHO (EC Clearinghouse,1993), as follows:
Oral candidiasis
Shiny erythematous areas of mucosa, sometimes with white patches interspersed. The four clinical subtypes are characterized as:
- Erythematous type: red area without removable white spots or plaques.
- Pseudomembranous type: white removable spots or plaques.
- Hyperplastic type: firm, adherent, unscrapable white plaques.
- Angular cheilitis: fiery red commissures with a fissuring or cracking appearance.
Oral hairy leukoplakia (OHL)
Non-scrapable, corrugated white plaques that did not respond to anti-fungal therapy. These were always on the lateral borders of the tongue.
Gingivitis
Distinctive dusky red, cyanosed free gingiva, presence of bleeding on probing and/or spontaneous bleeding.
HIV-gingivitis (Linear gingival erythema)
Gingiva which presents an unusual clinical appearance, such as fiery red band along the margin of the gingiva, with or without focal enlargement of the gingiva in an otherwise healthy oral cavity. No ulceration present, nor pockets or loss of attachment.
Periodontitis
Presence of pockets >4 mm in one or more sites. All teeth present were probed around the whole circumference with a blunt periodontal probe, with William’s markings.
Oral (melanin) pigmentation
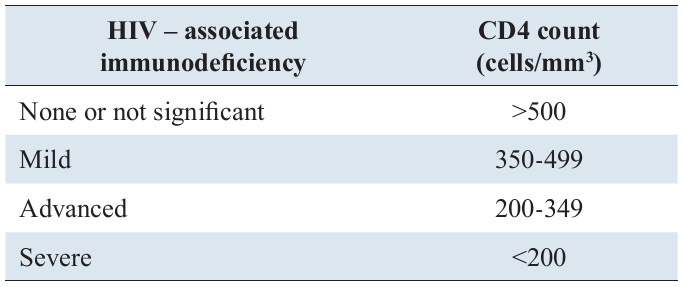
Brown/brownish-black, spotty/diffuse macules, usually occupy areas greater than 1 cm and asymmetrical in distribution. The level of immunosuppression in each patient was classified according to WHO immunologic staging (Table 1).
Data collection and statistical analysis:
The data was recorded and the presence of each lesion was noted, the information collected was then divided into four groups on the basis of immunological classification of WHO. This was a cross-sectional study and point prevalence of each lesion was calculated. Since the nature of data congregated was categorical, chi square test was used to find the relationship between the four groups. After obtaining chi square test value, p value was ascertained and the value of
Results
125 patients (mean age, 32 ± 7.7 years old; 52% males) were investigated. The mean duration of infection was 5.4 ± 3.2 years. Medical history indicated taking anti- tuberculosis medication (25%) and constant use of antibiotics (40%), anti-fungal therapy (4%) and highly active antiretroviral therapy (HAART, 44%).
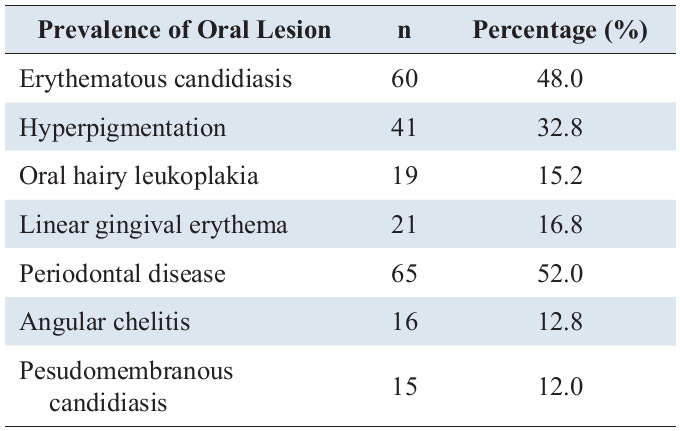
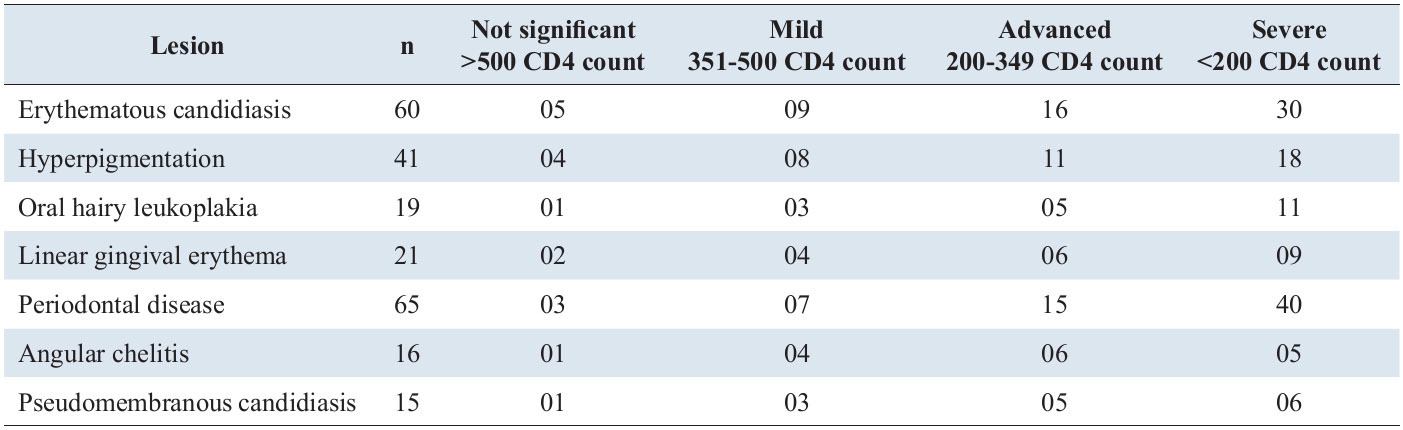
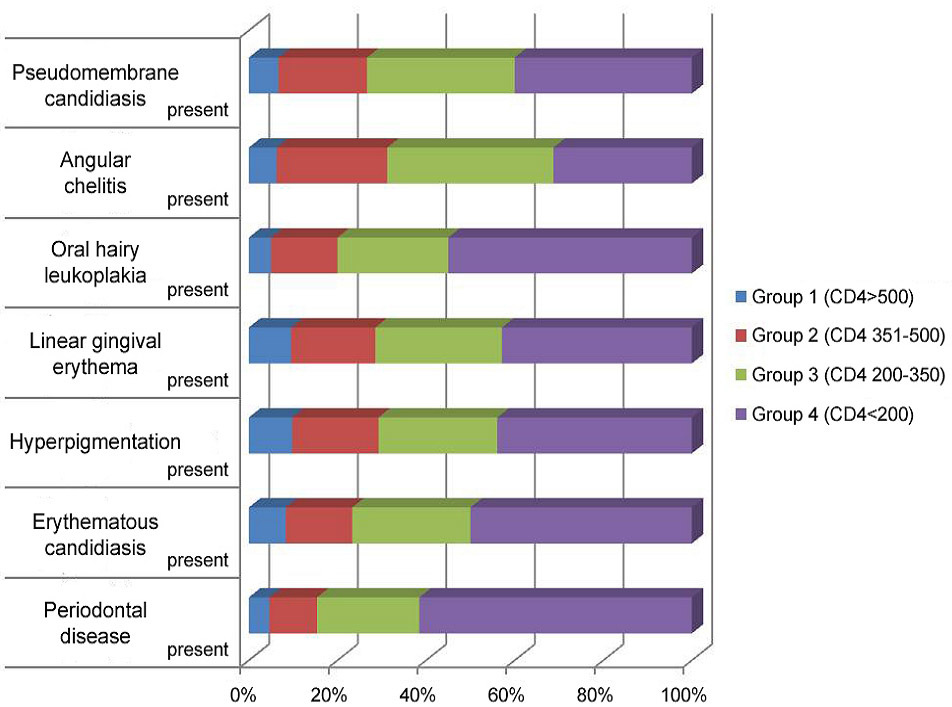
Absolute CD4 counts were categorized in four different groups: Group I (>500 cells/mm³), Group II (350-499 cells/mm³), Group III (200-349 cells/mm³) and Group IV (0-200 cells/mm³). Out of the 125 cases studied, it was observed that 60 patients (52%) of the cases exhibited periodontal disease which was highest prevalence of the oral lesions followed by erythematous candidiasis (48%). The pseudomembranous form of candidiasis was seen in 12% of the cases (Table 2).
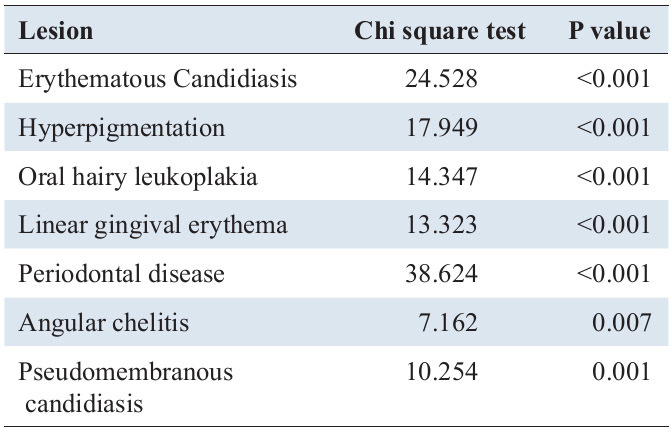
As the immunosuppression worsened the oral manifestations increased (Table 3). In groups 1-3 the most prevalent manifestation was erythematous candidiasis (chi square - 24. 528 and p
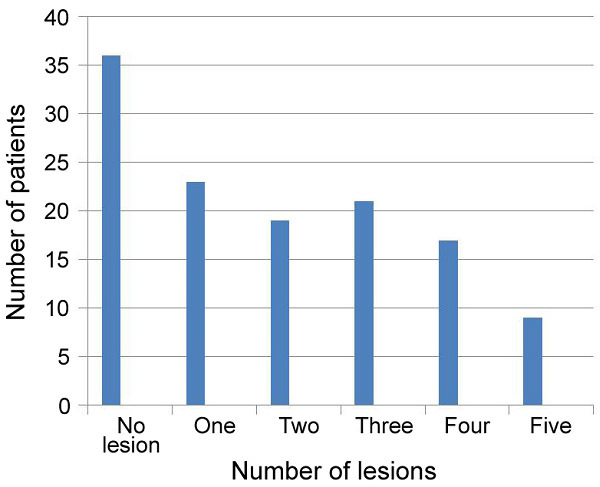
89 out of total 125 cases showed the presence of lesion, one lesion was observed in 23 patients, 2 in 19, 3 lesions in 21 cases, 4 in 17 patients and 5 lesions in 9 cases (Figure 1).
There was an evident increase in number of lesion and decreased average CD4 count with increased level of immunosuppression (Figure 2).
Discussion
Various studies have noted different prevalence of oral lesions due to variable sample size, degree of immunosuppression, inter-examiner differences, and regional patterns of infectious diseases. Therefore, extrapolating the results comparing the reported prevalence of existing studies may not be useful.
This study had almost equal gender distribution with 52% males which is in contrast to the studies done by Sharma et al. [
The study was done in the age group of 20-40 years as this age range shows the peak distribution of people affected with HIV.
The present study noted an overall prevalence of oral lesions of 71% in the HIV infected population of Dakshina Kannada regardless of the severity of the disease which is lower when compared to previous studies done by Sharma et al. [
Periodontal disease showed the highest prevalence (52%), which was not noted in the previous studies; this may be a result of poor oral hygiene, drugs, medications. Periodontitis showed highly significant relationship with the increase in immunosuppression.
Oral candidiasis was the common finding with Erythematous candidiasis showing prevalence in 48% of the patients which is in agreement with a previous study done in the same region by Sharma and colleagues [
The prevalence of oral lesions viz. hyperpigmentation (32.8%), linear gingival erythema (16.8%), hairy leukoplakia (15.2%), angular cheilitis (12.8%), and pseudomembranous candidiasis (12%) was found to be consistent with the previous studies [
With new research studies, the treatment modalities instituted have increased the lifespan of people infected with HIV. Yengopal et al. in 2007 found that Oral lesions associated with HIV infection negatively affect the oral health–related quality of life in infected patients [
A significant relation was found between oral lesions and the degree of immunosuppression (p value12]. The oral lesions were studied according to the immunosuppression staging done by WHO in 2007 so that the preventive measures instituted for the oral health can be correlated to the WHO treatment guidelines in different stages of infection. This may also have implications on diagnosis and prognosis of the disease [
The periodontal disease and oral hairy leukoplakia increased sharply in the severely immunosuppressed stage of HIV disease and can be useful in predicting the progression of the disease.
Even though, there is an increase in awareness, prevention and extensive treatment strategies due to the programmes carried out by WHO in developing countries, the decrease in oral lesions is not significant hence studies testing the methods of improving oral hygiene and in turn oral health needs to be carried out.
Acknowledgments
The authors would like to acknowledge Indian Council of Medical Research, New Delhi, India, ART centre, Wenlock Hospital and Nitte University, Mangalore.
References
- Bajpai S, Pazare AR . Oral manifestations of HIV. Contemp Clin Dent 2010; 1 (1): 1-5.
Reference Link - Little J, Falace D, Miller C, Rhodus NL. Dental Management of the Medically Compromised Patients, 6th ed. Laxington: Mosby; 2003; 221-222.
- Pedreira EN, Cardoso CL, Barroso Edo C, Santos JA, Fonseca FP, Taveira LA. Epidemiological and oral manifestations of HIV positive patients in a specialized service in Brazil. J Appl Oral Sci 2008; 16: 369-375.
Reference Link - Santos LC, Castro GF, De Souza IP, Oliveira RH. Oral manifestations related to immunosuppression degree in HIV positive children. Braz Dent J 2001; 12: 135-138.
- Flaitz CM, Hicks MJ. Oral candidiasis in children with immune suppression: clinical appearance and therapeutic considerations. ASDC J Dent Child 1999; 66: 161-6,154.
- Taiwo OO, Okeke EN, Jalo PH, Danfillo IS. Oral manifestation of HIV/AIDS in Plateau state indigenes, Nigeria West. Afr J Med 2006; 25: 32-37.
- Sud N, Shanker V, Sharma A, Sharma NL, Gupta M. Mucocutaneous manifestations in 150 HIV - infected Indian patients and their relationship with CD4 lymphocyte counts. Int J STD AIDS 2009; 20: 771-774.
Reference Link - Nokta M. Oral manifestations associated with HIV infection. Curr HIV/AIDS Rep 2008;5: 5-12.
Reference Link - EEC Clearinghouse on oral problems related to HIV infection and WHO Collaborating Center on oral manifestations of the Human Immunodeficiency Virus. Classification and diagnostic criteria for oral lesions in HIV infection. J Oral Pathol Med 1993; 22: 289-291.
Reference Link - World Health Organization WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV - related disease in adults and children. World Health Organization, Geneva: 1-52.
- Adurogbangba MI, Aderinokun GA, Odaibo GN, Olaleye OD, Lawoyin TO. Oro-facial lesions and CD4 counts associated with HIV/AIDS in an adult population in Oyo State, Nigeria. Oral Dis. 2004; 10: 319-326.
Reference Link - Sharma. G, Pai. KL, Shetty. S, Ramapuram JT, Nagpal A. Oral manifestations as predictors of immune suppression in a HIV ? AIDS infected population in South India. Clin Oral Invest. 2009; 13: 141-148.
- Sharma G, Pai KM, Suhas S, Ramapuram JT, Doshi D, Anup N. Oral manifestations in HIV / AIDS infected patients from India. Oral Dis. 2006; 12: 537-542.
Reference Link - Soares MSM, Leite DFBM, Arnaud RR, Filho FDCO, Lima AMH, De Sousa DS et al. Oral Lesions and systemic diseases in HIV - infected subjects. J. Infect. Dis. Immun. 2011; 3: 172-175.
- Yengopal V, Naidoo S. Do oral lesions associated with HIV affect quality of life? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 66-73.
Reference Link - K Ranganathan, M Umadevi, TR Saraswathi, N Kumaraswamy, S Solomon, N Johnson. Oral lesions and conditions associated with Human Immunodeficiency Virus infection. Ann Acad Med Singapore 2004; 33(Suppl): 37S-42S.
- Nittayananta W, Chungpanich S. Oral lesions in a group of Thai people with AIDS. Oral Diseases 1997; 3 (Suppl 1):41-56.
- Ranganathan K, Reddy BVR, Kumarasamy N, Solomom S, Viswanathan R, Johnson NW. Oral lesions and conditions associated with human immunodeficiency virus infection in 300 south Indian patients. Oral Diseases 2000; 6: 152-157.
Reference Link